Fillable Do Not Resuscitate Order Document for Texas
When a person decides they want to refuse certain life-saving treatments in the event of severe health emergencies, the Texas Do Not Resuscitate (DNR) Order form becomes a crucial document. This legal form communicates to medical professionals that an individual has chosen not to undergo procedures such as CPR (cardiopulmonary resuscitation) if their heart stops or they stop breathing. It's a decision that speaks volumes about an individual's desire for their end-of-life care and emphasizes the importance of respecting a person's healthcare wishes. Navigating the complexities of this form requires an understanding of its implications, from who can sign it to how it affects emergency medical services. The form is more than just a piece of paper; it is a declaration of personal healthcare preferences, ensuring that medical treatment aligns with the individual's wishes. Understanding the Texas Do Not Resuscitate Order form is essential for anyone looking to make informed decisions about their health care directives or those of their loved ones.
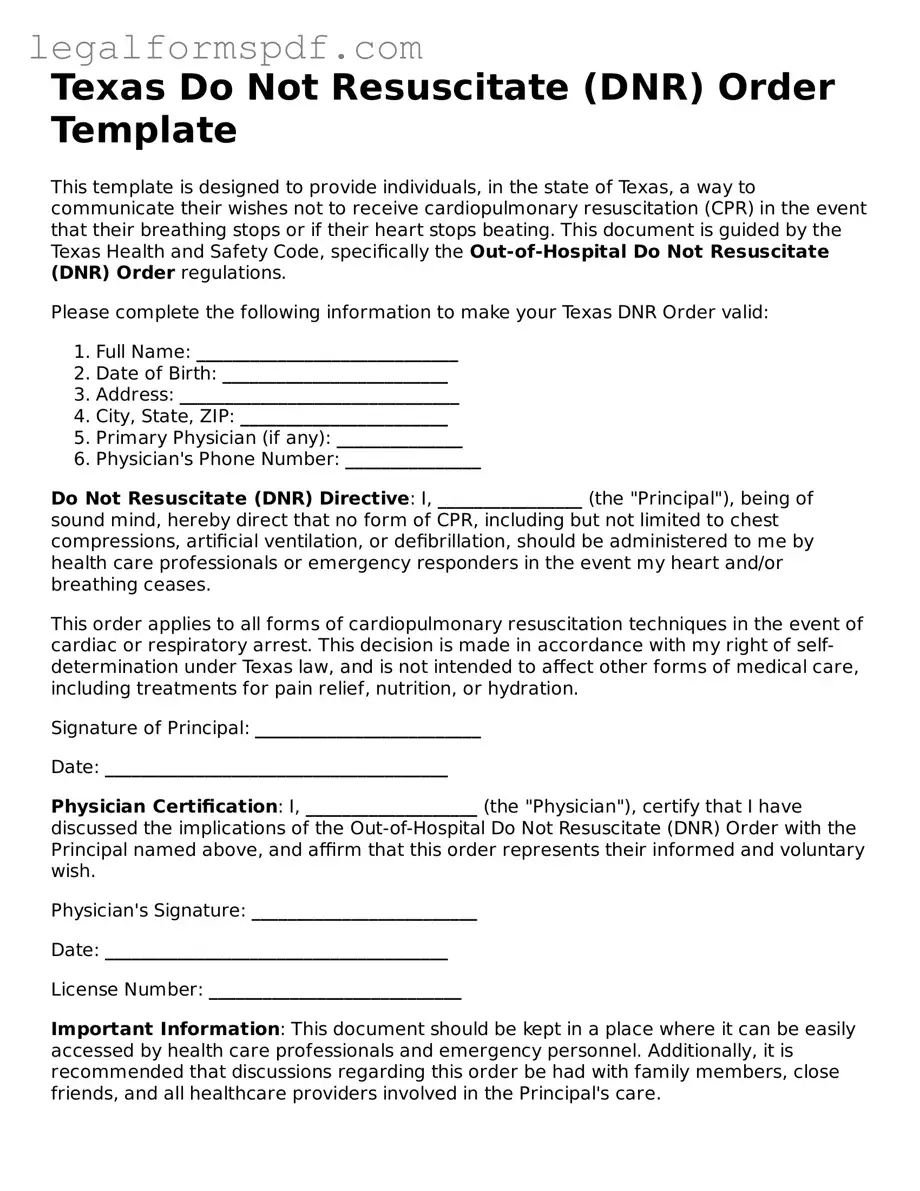
Document Example
Texas Do Not Resuscitate (DNR) Order Template
This template is designed to provide individuals, in the state of Texas, a way to communicate their wishes not to receive cardiopulmonary resuscitation (CPR) in the event that their breathing stops or if their heart stops beating. This document is guided by the Texas Health and Safety Code, specifically the Out-of-Hospital Do Not Resuscitate (DNR) Order regulations.
Please complete the following information to make your Texas DNR Order valid:
- Full Name: _____________________________
- Date of Birth: _________________________
- Address: _______________________________
- City, State, ZIP: _______________________
- Primary Physician (if any): ______________
- Physician's Phone Number: _______________
Do Not Resuscitate (DNR) Directive: I, ________________ (the "Principal"), being of sound mind, hereby direct that no form of CPR, including but not limited to chest compressions, artificial ventilation, or defibrillation, should be administered to me by health care professionals or emergency responders in the event my heart and/or breathing ceases.
This order applies to all forms of cardiopulmonary resuscitation techniques in the event of cardiac or respiratory arrest. This decision is made in accordance with my right of self-determination under Texas law, and is not intended to affect other forms of medical care, including treatments for pain relief, nutrition, or hydration.
Signature of Principal: _________________________
Date: ______________________________________
Physician Certification: I, ___________________ (the "Physician"), certify that I have discussed the implications of the Out-of-Hospital Do Not Resuscitate (DNR) Order with the Principal named above, and affirm that this order represents their informed and voluntary wish.
Physician's Signature: _________________________
Date: ______________________________________
License Number: ____________________________
Important Information: This document should be kept in a place where it can be easily accessed by health care professionals and emergency personnel. Additionally, it is recommended that discussions regarding this order be had with family members, close friends, and all healthcare providers involved in the Principal's care.
For any questions or more detailed information regarding the Texas DNR Order, please consult with a legal professional or healthcare provider.
PDF Specifications
| Fact Number | Detail |
|---|---|
| 1 | The Texas Do Not Resuscitate (DNR) Order Form is governed by Texas Health and Safety Code, Chapter 166. |
| 2 | This form allows individuals to decline certain life-sustaining treatments in the event of cardiac or respiratory arrest. |
| 3 | To be valid, the form must be signed by the patient or the patient's legally authorized representative. |
| 4 | A physician must also sign the form, agreeing to the patient's wishes not to receive specified treatments. |
| 5 | The Texas DNR Order is applicable in various settings, including hospitals, long-term care facilities, and at home. |
| 6 | For the DNR Order to be effective at home, it must be readily available and presented upon request to emergency personnel. |
| 7 | Electronic versions of the form held on smartphones or other devices may not be recognized by all emergency personnel. |
| 8 | Reversing a DNR Order requires a new order to be filled out and signed, revoking the previous directive. |
| 9 | Without a valid Texas DNR Order, medical personnel are required to attempt resuscitation in emergencies. |
| 10 | It is advisable to discuss the decision with healthcare providers and family members to ensure the patient's wishes are clearly understood and respected. |
Instructions on Writing Texas Do Not Resuscitate Order
A Do Not Resuscitate (DNR) Order in Texas is a critical document for individuals who wish to decline certain life-sustaining treatments in emergency medical situations. Completing this form requires careful attention to detail and a clear understanding of one's wishes regarding end-of-life care. Below, you'll find straightforward steps to help you accurately complete the Texas DNR Order form, ensuring your healthcare preferences are respected and legally recognized.
- Locate the official Texas Do Not Resuscitate Order form. This can typically be found online through Texas health-related governmental websites or at healthcare facilities.
- Read the form thoroughly before beginning to fill it out. Understanding each section will help ensure that you complete the form accurately and in accordance with your wishes.
- Enter the patient's full name at the top of the form where indicated. This should be the name of the individual the DNR Order applies to.
- Fill out the patient's date of birth and address in the designated areas. Accurate information here is crucial for identifying the patient correctly in emergency situations.
- Discuss the implications of the Do Not Resuscitate Order with a physician. The physician must explain what the DNR Order means and the specific treatments that will not be administered if the order is in place.
- After understanding all implications, the patient or the patient's legally authorized representative must sign the form. If the patient is unable to sign due to medical reasons, a representative who has the legal authority to make healthcare decisions for the patient can sign on their behalf.
- The attending physician must also sign the form, confirming that the patient (or their representative) understands the nature and the consequences of the DNR Order.
- Once completed, a copy of the Do Not Resuscitate Order should be kept with the patient’s medical records. It is also advisable to inform family members and other caregivers about the existence and location of the DNR Order.
Completing a Texas Do Not Resuscitate Order is a significant step in managing one’s healthcare preferences. By following these steps carefully, individuals can ensure that their wishes regarding life-sustaining treatments are known and respected in times of emergency. It's not just about filling out a document; it's about making a choice that aligns with your personal values and healthcare goals.
Understanding Texas Do Not Resuscitate Order
What is a Do Not Resuscitate Order (DNR) in Texas?
A Do Not Resuscitate Order, or DNR, is a medical order written by a doctor. It instructs health care providers not to perform cardiopulmonary resuscitation (CPR) if a patient's breathing stops or if the patient's heart stops beating. In Texas, this order is specifically tailored to respect the wishes of the patient regarding end-of-life care.
Who can request a DNR Order in Texas?
Any competent adult can request a DNR order for themselves in Texas. This includes patients with a terminal condition or irreversible condition as diagnosed by a physician. The decision can also be made by a legally authorized representative if the patient is unable to communicate their wishes due to their medical condition.
How is a DNR Order executed in Texas?
In Texas, a DNR Order must be signed by a physician to be valid. It should be discussed and executed with the patient's participation if possible, or with the patient's legally authorized representative. The order is then documented in the patient's medical records. It's important to note that the patient or their representative can obtain the form from their health care provider or the Texas Department of State Health Services (DSHS).
Can a DNR Order be revoked?
Yes, a DNR Order can be revoked at any time by the patient or their legally authorized representative. The revocation does not need to be in writing; it can be done verbally or through any clear indication that the patient wishes to withdraw the DNR order. Health care providers should be promptly informed about the revocation to ensure it is reflected in the patient's medical records.
Is there a specific form for DNR Orders in Texas?
Yes, Texas has a specific form for DNR Orders that must be used. This form is approved by the Texas Department of State Health Services and can be obtained from a healthcare provider or directly from the DSHS. The use of the official form ensures that the DNR order meets all the legal requirements set forth by the state of Texas.
What if a patient is transferred to another facility?
If a patient with a DNR Order is transferred to another facility, the order remains valid. It is crucial that the order, or a copy of it, accompanies the patient to the new facility. This helps ensure that the patient's wishes regarding resuscitation are respected across different care settings.
Does a DNR Order affect other treatments?
No, a DNR Order does not affect the provision of other medical treatments. The order specifically relates to CPR and does not prevent a patient from receiving other forms of medical care, such as pain management, oxygen, or other interventions aimed at providing comfort and support.
Where should a DNR Order be kept?
A DNR Order should be kept in a place where it can be easily found by healthcare providers, such as with the patient's medical records at home or if the patient resides in a healthcare facility, with their records there. It's also a good idea for the patient or their representative to inform family members and healthcare providers of the order's existence and location.
Common mistakes
Filling out a Texas Do Not Resuscitate (DNR) Order form requires careful attention to detail to ensure that the document is legally valid and reflects the wishes of the individual it concerns. A common mistake is not ensuring that the person for whom the DNR is intended (or their legally authorized representative) signs and dates the form. This step is crucial as it provides evidence of the individual's desire not to receive cardiopulmonary resuscitation (CPR) in the event that their breathing or heartbeat stops. Without a valid signature and date, healthcare providers may be legally obligated to perform CPR, even if it goes against the person's wishes.
Another error often made is overlooking the requirement for a physician's signature. A Texas DNR order must be signed by a licensed physician to be considered valid. This signature verifies that the physician has discussed the implications of a DNR order with the patient or their representative, ensuring that the decision is made with a clear understanding of the consequences. Failure to obtain a physician's signature renders the DNR form ineffective, potentially leading to unwanted medical interventions.
Many individuals also forget to distribute copies of the DNR order to relevant parties. Once the DNR form is completed and properly signed, it should be given to the patient's healthcare providers, including their primary care physician, specialists, and home health agency if applicable. In addition, keeping a copy in an easily accessible place at home is advisable in case emergency medical services (EMS) are called. Failure to disseminate the DNR order broadly can result in its directives being unknown and unheeded at a critical moment.
Lastly, a misunderstanding of the scope of a DNR order is a frequent issue. Some believe that a DNR order restricts all forms of medical intervention. However, it specifically applies to CPR and does not affect other treatments, such as pain relief, nutrition, hydration, or the administration of medication. Clarifying the limitations and implications of a DNR order can prevent misinterpretations that could affect the individual's healthcare in unforeseen ways.
Documents used along the form
In the context of planning and communicating end-of-life wishes, the Texas Do Not Resuscitate (DNR) Order form is a crucial document. However, it is often one of several essential forms and documents that work together to ensure a person's healthcare preferences are fully respected and legally recognized. Alongside a Texas DNR, individuals typically consider preparing additional legal documents to create a comprehensive end-of-life care plan. Below are eight such forms and documents commonly used in conjunction with the Texas DNR Order form.
- Medical Power of Attorney (MPOA): This document allows an individual to appoint someone they trust to make healthcare decisions on their behalf if they become incapable of making those decisions themselves.
- Advance Healthcare Directive (Living Will): This legal document outlines specific medical treatments an individual wants or does not want if they become seriously ill and are unable to communicate their wishes.
- HIPAA Release Form: The Health Insurance Portability and Accountability Act (HIPAA) Release Form grants permission for healthcare providers to discuss an individual's medical information with designated persons.
- Out-of-Hospital Do Not Resuscitate (OOH-DNR) Order: Similar to a traditional DNR, the OOH-DNR is specifically designed for use outside of hospital settings, including at home or in hospice care, to prevent emergency medical personnel from initiating resuscitation.
- Directive to Physicians and Family or Surrogates: This document, also known as a Living Will, allows individuals to communicate their wishes regarding the use of life-sustaining treatments if they are diagnosed with a terminal or irreversible condition.
- Declaration for Mental Health Treatment: This legal form lets individuals make decisions in advance about mental health treatment, including preferences about medications, electroconvulsive therapy (ECT), and admittance to mental health facilities for a limited duration.
- Physician Orders for Scope of Treatment (POST): This medical order details a patient’s preferences for treatments such as antibiotics, IV fluids, and intubation. It is intended for those with serious illnesses or at the end of life.
- Last Will and Testament: While not directly related to healthcare decisions, a Last Will and Testament is critical for outlining how an individual’s assets and personal matters should be handled after death.
Together with the Texas DNR Order, these documents contribute to a well-rounded and legally sound approach to end-of-life planning. In preparing these documents, individuals can ensure their healthcare wishes are recognized and respected, while also providing clarity and guidance to their loved ones and healthcare providers. It's advisable to consult with legal and healthcare professionals when preparing these documents, to ensure they are correctly executed and reflect the individual’s wishes accurately.
Similar forms
A Living Will, also known as an advance healthcare directive, bears similarity to the Texas Do Not Resuscitate (DNR) Order in several respects. Both documents allow individuals to make their healthcare preferences known in advance, including decisions regarding life-sustaining treatments. Unlike a DNR, which specifically declines resuscitation efforts in the event of cardiac or respiratory arrest, a living will covers a broader range of medical interventions and scenarios, offering detailed instructions on the person's wishes concerning medical treatment in various situations where they are unable to communicate.
The Medical Power of Attorney (POA) is another document that shares common ground with a DNR. It grants a designated agent the authority to make healthcare decisions on behalf of the individual, should they become incapacitated and unable to make such decisions for themselves. While a Medical POA covers a wide array of health care decisions, a DNR is specific to the act of not administering CPR if the person's breathing or heart stops, highlighting the specificity of a DNR's scope in comparison to the broader authority granted by a Medical POA.
The POLST form, or Physician Orders for Life-Sustaining Treatment, is akin to a DNR in its focus on end-of-life care decisions, specifically those made in anticipation of a medical emergency. Both are medical orders that are signed by a healthcare provider and directly inform medical personnel of a patient's choices regarding life-sustaining treatments, including CPR. However, POLST forms go beyond DNR orders by addressing a wider range of interventions such as hospitalization, antibiotics, and artificial nutrition and hydration.
Patient Self-Determination Act (PSDA) documents, required by federal law for all individuals admitted to a healthcare facility, also share a connection with DNRs. These documents are designed to inform patients of their rights to make decisions regarding their medical care, including the right to accept or refuse medical or surgical treatment and the right to prepare an advance directive. Similarly, a DNR order is a form of advance directive that specifically relates to the refusal of cardiopulmonary resuscitation in emergencies.
Lasting, a HIPAA Release Form, while primarily focused on the privacy and release of medical information, intersects with the purpose of a DNR in the sphere of personal healthcare management. By authorizing the disclosure of one's medical information to designated individuals, it enables informed decisions regarding a patient's healthcare, including the enforcement of a DNR order. The connection here lies in the facilitation of communication about a patient's wishes among healthcare providers, the patient, and potentially their appointed agents or family members, ensuring that the patient's healthcare preferences, such as those expressed in a DNR, are respected and followed.
Dos and Don'ts
Filling out a Texas Do Not Resuscitate (DNR) Order form is a critical step for ensuring that an individual's wishes regarding resuscitation are respected. To ensure that the DNR order is properly completed and legally valid, it is important to follow certain guidelines. Here is a list of things you should and shouldn't do:
- Do make sure the person for whom the DNR is being prepared is fully informed about what a DNR order means.
- Do consult with a healthcare provider to ensure the form is properly explained and understood.
- Do ensure that the form is filled out completely, leaving no sections blank unless specifically instructed.
- Do use a blue or black ink pen when filling out the form to ensure legibility and prevent potential issues with photocopies or scans.
- Do verify that the individual's name on the DNR form matches the name on their identification and medical records exactly.
- Don't forget to have the form signed by the required parties, which typically include the patient (or their legally authorized representative) and the physician.
- Don't leave the form at home; make sure it is easily accessible to emergency responders, such as in a visible location within the residence or registered with a local hospital or physician's office.
- Don't alter the form after it has been signed without proper legal and medical consultation. If changes are necessary, a new form should be completed, signed, and dated.
- Don't hesitate to ask questions. If there's any confusion or concern about the form or its implications, seek clarification from medical professionals or legal advisors.
Misconceptions
The Texas Do Not Resuscitate (DNR) Order is a critical legal document, yet subject to widespread misconceptions. It's imperative to clarify these misunderstandings to ensure individuals can make informed decisions about their healthcare. Below are five common misconceptions about the Texas DNR Order form, meticulously corrected for better understanding.
It applies to all medical treatments: A common fallacy is the belief that a Texas DNR Order restricts all forms of medical treatment. In truth, this document specifically addresses the refusal of cardiopulmonary resuscitation (CPR) in the event that a person's heart stops or they stop breathing. It does not preclude a person from receiving other types of medical care, such as pain management, oxygen, or other non-invasive treatments that can provide comfort and support.
It's only for the elderly: Another misconception is that DNR Orders are exclusively for older adults. In reality, these orders are important for people of any age who have a serious illness, are in a condition where CPR would not be successful, or have decided, for personal or medical reasons, that they would not want CPR attempted should their heart or breathing stop. The decision to have a DNR Order is deeply personal and can be relevant for individuals across the lifespan.
Doctor's approval is not needed: Some people wrongly assume that they can enact a DNR Order without consulting a healthcare provider. However, in Texas, for a DNR Order to be legally valid, it must be signed by a physician. This measure ensures that the patient fully understands the implications of the order and that it aligns with their current health status and end-of-life wishes.
A DNR Order is permanent: It’s a common belief that once a DNR Order is placed, it is irreversible. Nevertheless, individuals have the right to change their minds at any time. A Texas DNR Order can be revoked or amended according to the patient's wishes. Open and ongoing communication with healthcare providers is crucial to ensure that the DNR Order reflects the patient's current preferences.
It's only for hospital use: Many assume that a DNR Order is applicable only within hospital settings. The reality is, in Texas, a DNR Order can be effective both in healthcare facilities and in non-institutional settings such as the patient’s home. This flexibility allows patients to make known their preference not to receive CPR in a wide range of environments, enhancing their autonomy and control over end-of-life care decisions.
Understanding these key aspects of the Texas Do Not Resuscitate Order form empowers individuals and their families to make informed choices that align with their healthcare goals and personal values. It underscores the importance of thoughtful discussions with healthcare providers and loved ones about end-of-life care preferences.
Key takeaways
Individuals in Texas have the right to make informed decisions about their medical treatments, including the choice not to receive resuscitation in the event of cardiac or respiratory arrest. This decision is formalized through the Texas Do Not Resuscitate (DNR) Order form.
The Texas DNR Order form must be completed by a qualified patient or their legally authorized representative, along with a physician, who agrees that resuscitation should not be attempted.
It is important to ensure that the form is filled out accurately and completely to avoid any ambiguity regarding the patient's wishes. All required sections and signatures must be completed for the form to be legally valid.
The DNR Order form should be kept in a place where it is easily accessible to emergency medical personnel, such as with the patient, in their home, and in their medical records.
Emergency medical services and healthcare providers are legally obligated to respect the wishes documented in a valid Texas DNR Order, given the form is present and accessible during an emergency.
Communication is crucial. Patients are encouraged to discuss their decision with family, caregivers, and healthcare providers to ensure that everyone involved is aware of their wishes regarding life-saving measures.
It is possible to rescind or revoke a DNR Order at any time. To do so, the patient or their authorized representative must inform their healthcare provider of their change in decision. Additionally, physically destroying the DNR Order form can serve as a means to revoke it.
The Texas DNR Order does not expire. However, it is advisable to revisit and discuss the order periodically with healthcare providers to ensure that it continues to reflect the patient's current wishes.
More Do Not Resuscitate Order State Forms
Does a Dnr Need to Be Notarized in California - A Do Not Resuscitate Order (DNR) is a legal document that instructs healthcare providers not to perform CPR if a patient's breathing stops or if the heart ceases beating.
Printable Dnr Form - Reviewing and updating a DNR Order is important, especially if a patient's health status or wishes change over time.
Il Polst Form - The form can be revoked or updated at any time by the patient, as long as they are mentally competent to make such a decision.