Fillable Do Not Resuscitate Order Document for North Carolina
In the state of North Carolina, individuals have the right to make decisions about their healthcare, especially when it comes to the topic of life-saving treatments in critical moments. One significant aspect of exercising this right involves the use of a Do Not Resuscitate (DNR) Order form. This legal document communicates a person's wish to forego CPR (cardiopulmonary resuscitation) or advanced cardiac life support (ACLS) if their heart stops beating or they stop breathing. It's especially pertinent for patients with serious illnesses or those in advanced age who seek to avoid aggressive interventions at the end of life. The form must be filled out accurately and signed by the individual (or their legal healthcare representative) and their physician to ensure its validity. This document then serves as a critical guide for healthcare providers, ensuring that the patient's wishes are respected in emergency situations. By understanding the major aspects of the North Carolina Do Not Resuscitate Order form and its profound implications for one’s end-of-life care, individuals can take significant steps towards ensuring their medical care aligns with their personal values and preferences.
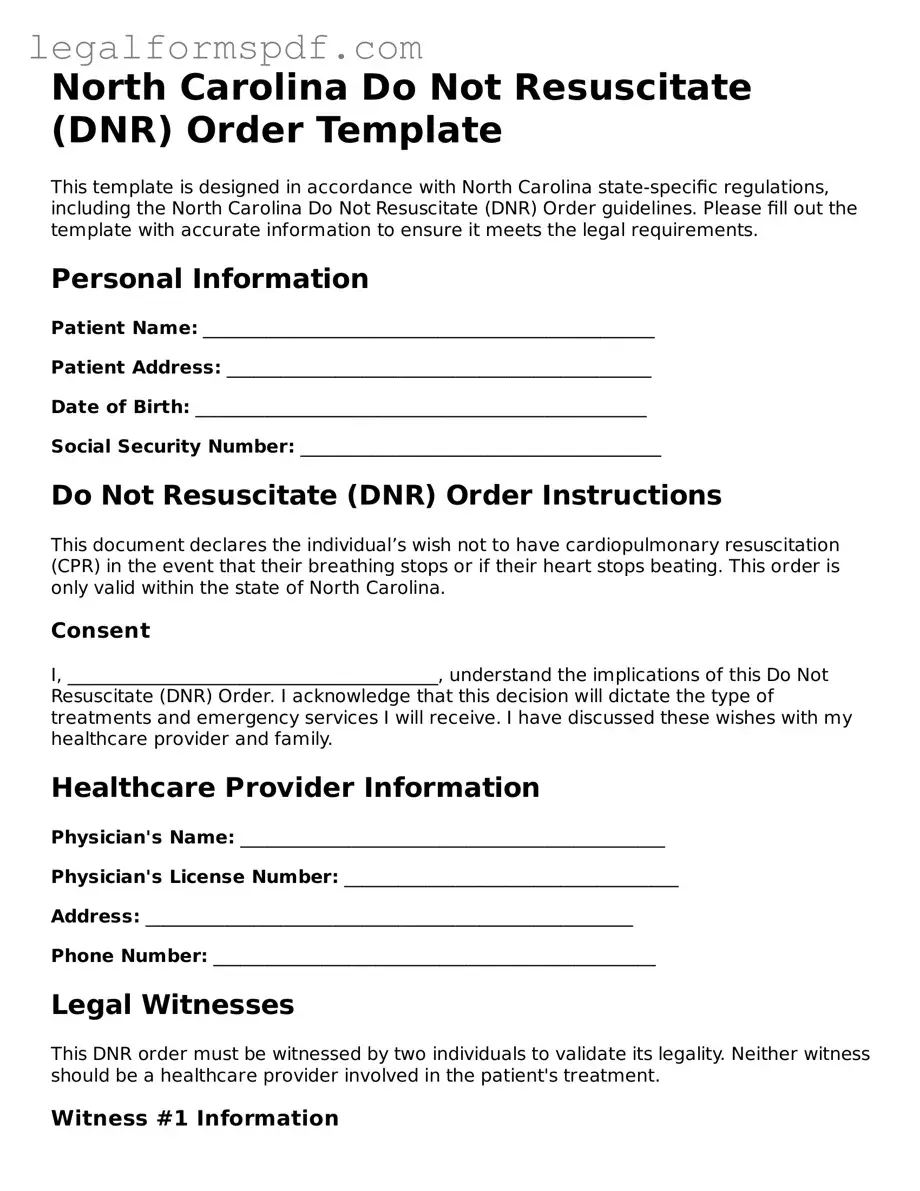
Document Example
North Carolina Do Not Resuscitate (DNR) Order Template
This template is designed in accordance with North Carolina state-specific regulations, including the North Carolina Do Not Resuscitate (DNR) Order guidelines. Please fill out the template with accurate information to ensure it meets the legal requirements.
Personal Information
Patient Name: __________________________________________________
Patient Address: _______________________________________________
Date of Birth: __________________________________________________
Social Security Number: ________________________________________
Do Not Resuscitate (DNR) Order Instructions
This document declares the individual’s wish not to have cardiopulmonary resuscitation (CPR) in the event that their breathing stops or if their heart stops beating. This order is only valid within the state of North Carolina.
Consent
I, _________________________________________, understand the implications of this Do Not Resuscitate (DNR) Order. I acknowledge that this decision will dictate the type of treatments and emergency services I will receive. I have discussed these wishes with my healthcare provider and family.
Healthcare Provider Information
Physician's Name: _______________________________________________
Physician's License Number: _____________________________________
Address: ______________________________________________________
Phone Number: _________________________________________________
Legal Witnesses
This DNR order must be witnessed by two individuals to validate its legality. Neither witness should be a healthcare provider involved in the patient's treatment.
Witness #1 Information
Name: __________________________________________________________
Address: ______________________________________________________
Phone Number: _________________________________________________
Witness #2 Information
Name: __________________________________________________________
Address: ______________________________________________________
Phone Number: _________________________________________________
Signature
By signing below, I verify that the information provided is accurate and that I comply with the guidelines provided by the state of North Carolina for a Do Not Resuscitate Order.
Patient Signature: ______________________________________________
Date: ___________________________________________________________
Physician Signature: ____________________________________________
Date: ___________________________________________________________
PDF Specifications
| Fact No. | Detail |
|---|---|
| 1 | The North Carolina Do Not Resuscitate (DNR) Order form is used by patients who wish not to receive CPR (Cardiopulmonary Resuscitation) in the event their heart stops or they stop breathing. |
| 2 | This form is part of a patient's advance directives, which are legal documents that guide decisions about healthcare when a person is unable to convey their wishes. |
| 3 | To be valid, the DNR order must be signed by a licensed healthcare provider in North Carolina. |
| 4 | The DNR order is recognized and respected across healthcare settings within North Carolina, including hospitals, nursing homes, and by emergency medical services (EMS). |
| 5 | Patients who decide to have a DNR order should inform their family members and healthcare providers to ensure the order is followed properly. |
| 6 | The form is governed by North Carolina General Statutes, particularly Article 23 of Chapter 90, which deals with life-prolonging measures. |
| 7 | Having a DNR order does not affect the quality of care a patient receives and it is strictly followed only in cases where resuscitation is required. |
| 8 | It is important for the DNR order to be easily accessible to healthcare providers, especially in emergency situations where immediate decisions are needed. |
Instructions on Writing North Carolina Do Not Resuscitate Order
Completing a North Carolina Do Not Resuscitate (DNR) Order form is a step taken to ensure that an individual's medical treatment preferences are honored during critical health situations. This document communicates to healthcare providers that the person does not wish to receive cardiopulmonary resuscitation (CPR) in the event their heart stops or they stop breathing. It's a decision that requires careful consideration and discussion with healthcare professionals and loved ones. Once ready to fill out this order, follow these steps to ensure your wishes are clearly stated and officially recorded.
- Begin by gathering all necessary personal information, including your full legal name, date of birth, and address. This ensures that the healthcare team can accurately identify you.
- Consult with your primary care physician or a healthcare provider authorized to sign the DNR order in North Carolina. Discuss your decision thoroughly to ensure it aligns with your healthcare goals and wishes.
- Fill in your personal information in the designated sections of the form. Make sure to write legibly if filling out by hand or ensure clarity if the form is being typed.
- Review the form with your healthcare provider to confirm that the medical information, including your health condition that warrants a DNR order, is accurately documented.
- Both you (or your legally authorized representative if you are unable to sign yourself) and your healthcare provider must sign the form, acknowledging your wish not to receive CPR and verifying the medical advice received.
- After signing, make several copies of the DNR order. Keep the original with your important papers, provide a copy to your healthcare provider to be included in your medical records, and consider giving copies to close family members or caretakers.
- Finally, if you reside in a facility, such as a nursing home, ensure that they have a copy of your DNR order on file. This ensures that all care teams are aware of your wishes.
Following these steps carefully will facilitate the correct filing of your North Carolina DNR order. It's important to regularly review this document, especially if your medical condition changes, to ensure it continues to reflect your current healthcare preferences. Involving your family and healthcare provider in these discussions can also provide support and clarity on your healthcare decisions.
Understanding North Carolina Do Not Resuscitate Order
What is a Do Not Resuscitate Order form in North Carolina?
A Do Not Resuscitate (DNR) Order form in North Carolina is a legal document that tells healthcare providers not to perform CPR (cardiopulmonary resuscitation) if a person's breathing or heartbeat stops. This form is used by individuals who have decided, often due to a terminal illness or desire for a natural death, that they do not want resuscitative efforts if they are near death.
Who can request a DNR Order in North Carolina?
Adult individuals with the capacity to make healthcare decisions, or their legally authorized representative if the individual is unable to make decisions for themselves, can request a DNR Order. Healthcare providers, including physicians, can also suggest a DNR Order as part of discussing end-of-life care options with patients and their families.
How can one obtain a DNR Order?
To obtain a DNR Order in North Carolina, an individual or their representative must have a discussion with a healthcare provider. The healthcare provider must assess the individual's condition and agree that a DNR Order is appropriate. The order must then be signed by a licensed physician, physician assistant, or nurse practitioner to be valid.
Is the DNR Order form the same as a living will or healthcare power of attorney?
No, the DNR Order form is not the same as a living will or a healthcare power of attorney. The DNR specifically relates to the non-administration of CPR in the event of cardiac or respiratory arrest. A living will expresses a person's wishes about their medical treatment in various situations, while a healthcare power of attorney designates someone to make healthcare decisions on behalf of the individual if they are unable.
Where should the DNR Order be kept?
The DNR Order should be kept in a place where it can be easily accessed by emergency responders or healthcare providers, such as with the individual's other important documents or in a visible location within the home. It may also be helpful to inform family members, close friends, and caregivers of the location and existence of the order.
Can a DNR Order be revoked or changed?
Yes, a DNR Order in North Carolina can be revoked or changed at any time by the individual for whom it was issued or their legally authorized representative. To revoke or alter it, they must communicate their wishes to their healthcare provider. The healthcare provider should then document the revocation or change in the individual's medical records and ensure that the original DNR Order is destroyed or clearly marked as revoked.
Does having a DNR Order affect the quality of healthcare one receives?
Having a DNR Order does not affect the quality of healthcare an individual receives. It only instructs healthcare providers not to perform CPR in the event of cardiac or respiratory arrest. Individuals with a DNR Order will still receive all other appropriate treatments and palliative care to manage symptoms and maintain comfort.
Common mistakes
Filling out the North Carolina Do Not Resuscitate (DNR) Order form involves clear and precise communication between individuals and healthcare professionals. However, mistakes can occur, leading to misunderstandings or errors that impact the person's medical treatment preferences. One common mistake is not ensuring that the form is signed by both the patient (or their legally authorized representative) and the physician. This signature is vital as it validates the DNR order and legally binds healthcare providers to follow it.
Another mistake involves not using the patient's full legal name on the document. It's essential to avoid nicknames or abbreviations, as they can cause confusion in emergency situations, potentially leading to the misidentification of the patient. Similarly, incorrectly filling out the patient's date of birth or other identifying information can delay or complicate the recognition of the DNR order by emergency responders or hospital staff.
Often, individuals fail to discuss their DNR order with family members or caregivers, leading to surprise or conflict when the order is presented in an emergency. This oversight can cause additional stress during critical moments and may result in attempts to overturn the DNR order, especially if family members were unaware of the patient's wishes.
Keeping the DNR order in an obscure location is also a frequent error. The DNR order should be easily accessible, not tucked away in a safe or file cabinet. Emergency personnel must have immediate access to this document for it to be effective. A copy should also be provided to the individual’s primary healthcare provider to be incorporated into their medical records.
Some people make the mistake of not reviewing and updating their DNR order regularly. Changes in health status or personal wishes regarding end-of-life care necessitate updates to the DNR order. Without regular review, the order may not accurately reflect the current wishes of the individual.
A lack of clarity in expressing desires within the form itself is a challenge as well. The form should precisely reflect the individual's wishes regarding resuscitation and end-of-life care. Any ambiguity can lead to uncertainty among healthcare providers about how to proceed in an emergency situation.
Inaccuracies or inconsistencies in the documentation provided by physicians, such as incorrect patient information or failure to specify the conditions under which the DNR order should be applied, can render the document void. Therefore, it’s critical that the physician double-checks the information for accuracy.
Not making multiple copies of the signed DNR order is another oversight. Apart from keeping the original document in an accessible location, copies should be given to close family members, caregivers, and healthcare proxies. This ensures that the DNR order can be quickly presented when necessary.
Failing to understand the legal and medical implications of a DNR order is a significant error. Individuals should seek counsel from healthcare professionals or legal advisors to fully understand how a DNR order functions within North Carolina laws and how it will affect emergency medical treatment.
Lastly, not incorporating the DNR order into a broader advance care plan is a lost opportunity for ensuring that all aspects of a person's end-of-life wishes are understood and respected. The DNR order is an important element, but it should be part of a comprehensive approach that includes living wills, healthcare power of attorney, and clear communication with loved ones about one’s health care preferences.
Documents used along the form
When preparing for medical and end-of-life arrangements, individuals in North Carolina may consider several forms in addition to the Do Not Resuscitate (DNR) Order. These documents ensure that a person's healthcare preferences are known and respected, especially during times when they cannot communicate their wishes. The DNR Order is a critical component, but it's part of a broader spectrum of advance care planning documents.
- Health Care Power of Attorney - This legal document allows an individual to appoint another person, known as a health care agent, to make medical decisions on their behalf if they are incapable of doing so. This includes decisions beyond the scope of a DNR order.
- Living Will - Also known as an advance directive, a living will enables individuals to outline their preferences for medical treatment in specific situations where recovery is not expected. It acts as a guide for family members and healthcare providers.
- Medical Orders for Scope of Treatment (MOST) - This form complements a DNR order by providing detailed instructions about other types of end-of-life care preferences, including intubation, antibiotic use, and feeding tubes.
- Five Wishes Document - A comprehensive planning tool that allows individuals to express their personal, medical, and spiritual wishes. Unlike a traditional living will, it addresses aspects of comfort care, dignity, and how individuals wish to be treated by their caregivers and families.
- Organ and Tissue Donation Form - This form records an individual's wishes regarding organ and tissue donation after death. It is important for ensuring that these wishes are known and can be acted upon promptly.
- Emergency Medical Services (EMS) DNR Form - Specifically designed for emergency medical services, this form indicates that in the event of a cardiac or respiratory arrest, resuscitation efforts should not be attempted. It is particularly useful for individuals residing in nursing homes or under home care.
Together, these documents provide a comprehensive framework for healthcare planning, ensuring that all aspects of an individual’s care preferences are documented and can be honored. In North Carolina, it's advisable to discuss these documents with healthcare providers and a legal advisor to ensure that they accurately reflect one's wishes and are properly executed.
Similar forms
The North Carolina Do Not Resuscitate (DNR) Order form is similar in nature to a Living Will, as both documents pertain to an individual's preferences regarding medical treatments and interventions. A Living Will specifically outlines which life-sustaining treatments a person would or wouldn't want if they become unable to communicate their wishes due to a serious illness or incapacitation. Like a DNR, it is a directive to medical professionals about the patient's choices for end-of-life care, focusing broadly on treatments like mechanical ventilation or tube feeding, rather than the narrower focus on not initiating CPR.
Comparable to a DNR Order is a Medical Power of Attorney (POA), which allows an individual to designate another person to make healthcare decisions on their behalf if they are unable to do so. While a Medical POA covers a broad range of medical decisions, including the acceptance or refusal of treatments, medications, and procedures, a DNR specifically directs healthcare providers not to perform CPR. The designated agent in a Medical POA could make the decision to implement a DNR order based on the incapacitated individual's preferences and best interests.
A Physician Orders for Life-Sustaining Treatment (POLST) form is another document similar to a DNR in that it provides specific instructions for health care providers regarding a range of life-sustaining treatments based on the patient's current health condition. The POLST form goes beyond the DNR's focus on CPR to include patient preferences on other interventions such as hospitalization, intubation, and use of antibiotics or feeding tubes. This document is typically used by individuals with serious health conditions or those who are at the end of life.
An Advance Directive is a broader term that encompasses various types of healthcare directives, including both Living Wills and DNR orders. It is designed to communicate an individual's wishes regarding medical treatment in the event they become incapable of making or communicating decisions. While a DNR order specifically addresses the issue of CPR, advance directives can cover a wide range of medical decisions and treatments, including preferences for end-of-life care and the designation of a healthcare power of attorney.
The Emergency Medical Services (EMS) Do Not Resuscitate form is specifically designed to inform emergency medical personnel not to initiate resuscitation efforts. This document is closely related to the hospital-issued DNR order but is intended for use outside the hospital setting, such as at home or in a care facility. The EMS DNR ensures that an individual's wishes regarding CPR are respected by first responders and emergency medical technicians, similar to how a hospital DNR functions within a hospital or healthcare facility environment.
Dos and Don'ts
Filling out a North Carolina Do Not Resuscitate (DNR) Order form is an important step for those who wish to have their preferences known regarding CPR (cardiopulmonary resuscitation) in the event of a cardiac or respiratory arrest. Below are the dos and don'ts to consider when completing this form:
- Do consult with your healthcare provider before you decide. It’s crucial to understand the implications of a DNR order.
- Do ensure that all information is accurate and legible. This includes your full name, date of birth, and other personal details.
- Do discuss your decision with family members or those close to you. It's important they understand your wishes.
- Do have the form signed by a physician. North Carolina law requires a physician's signature for the DNR order to be valid.
- Do make multiple copies. Keep the original document in a safe but accessible place, and give copies to family members or caregivers.
- Don’t fill out the form if you have any doubts or unanswered questions. Speak to your healthcare provider to get clarity.
- Don’t leave blank spaces. If a section does not apply, consider marking it as "N/A" to indicate it's not applicable.
- Don’t use pencil or erasable ink. Fill out the form in black or blue ink to ensure permanence and legibility.
- Don’t forget to review and update the form periodically. Your desires regarding medical treatment may change over time.
Misconceptions
Understanding the North Carolina Do Not Resuscitate (DNR) Order form is crucial, yet several misconceptions often cloud its true purpose and application. These misunderstandings can lead to confusion and anxiety among patients and their families. Here, we aim to clarify some of the most common misconceptions.
- All healthcare providers instantly recognize and honor DNR orders. While medical professionals should respect these orders, in emergency situations, first responders might not be aware of a DNR. It's important to ensure that DNR orders are easily accessible and communicated to all healthcare providers involved in the patient's care.
- DNR orders apply to all medical treatments. This is not the case. DNR orders specifically apply to the withholding of CPR (cardiopulmonary resuscitation) in the event of cardiac or respiratory arrest. They do not affect other treatments or care that might be necessary for the patient's health and comfort.
- Having a DNR means you'll receive less medical care. Some might worry that a DNR order could influence the overall level of care provided. However, these orders only guide actions in the case of cardiac or respiratory arrest, not the entirety of medical care a patient receives.
- Only elderly patients can have DNR orders. Age is not a criterion for a DNR order. Patients of any age with chronic illnesses or in poor health, who wish to avoid aggressive life-saving measures, can discuss the option of a DNR with their healthcare provider.
- DNR orders are permanent and cannot be changed. Patients and their healthcare proxies have the right to revisit and revise their DNR orders at any time. These decisions should reflect the patient's current health status and personal wishes.
- Family members can override a DNR order. In North Carolina, once a DNR order is in place and properly signed, family members cannot override it unless they have legal authority and evidence that the patient's wishes have changed. This legal authority typically comes from being designated as a healthcare power of attorney.
- DNR orders must be reviewed and renewed annually. Unlike some medical orders that have expiry dates or require regular renewal, DNR orders remain in effect until they are rescinded or the patient passes away. However, it is a good practice to review these documents periodically to ensure they still reflect the patient's wishes.
Addressing these misconceptions head-on helps in ensuring that individuals make informed decisions about DNR orders in North Carolina. For anyone considering a DNR, it's advisable to communicate openly with healthcare providers and loved ones to ensure that their wishes are clearly understood and respected.
Key takeaways
The North Carolina Do Not Resuscitate (DNR) Order form is a document that is critically important for individuals who wish to make clear decisions about the type of medical care they want to receive in emergency situations, particularly in regards to not receiving cardiopulmonary resuscitation (CPR). Here are some key takeaways to understand when filling out and using this form:
- Eligibility Requirements: A DNR Order is available to any individual who, in consultation with their healthcare provider, decides that they do not want to receive CPR in the event of cardiac or respiratory arrest. This decision is often made by individuals with serious, life-limiting illnesses or those who wish to avoid aggressive life-prolonging treatments.
- Medical Professional Involvement: The form must be completed in conjunction with a licensed healthcare provider. This requirement ensures that the individual's medical condition warrants the issuance of a DNR Order and that the patient fully understands the implications of their decision.
- Clear Identification: Once completed, the DNR Order should be kept in a location where it can be easily found by emergency responders, such as with the individual, in a prominent place in the home, or registered in a state database if applicable. In some cases, individuals might also wear a DNR bracelet or necklace for easy identification.
- Legally Binding: The DNR Order is a legally binding document, meaning that healthcare providers and emergency personnel must follow the instructions outlined in the form as long as it can be presented at the time of need. Without a DNR Order, medical personnel will typically proceed with all life-saving measures, including CPR.
- Revocability: It's important to note that a DNR Order can be revoked by the individual at any time should they change their mind. The revocation process can be as simple as telling a healthcare provider of their wish to revoke the order or physically destroying the DNR form and any identifiers like bracelets or necklaces.
Understanding these key points ensures that individuals making decisions about a DNR Order do so with full knowledge of its implications and the process involved. It's a significant step in managing one's health care wishes and ensuring they are respected.
More Do Not Resuscitate Order State Forms
Dnr Directive - Documentation confirming an individual's decision not to undergo CPR in life-threatening conditions.
Dnr Form Ohio - Encourages thoughtful conversation about end-of-life care preferences, promoting individual autonomy.
Dnr Form Georgia - A sensitive but necessary component of planning for those with terminal illnesses or in advanced age.
How Old Do You Have to Be to Sign a Dnr - Critical for ensuring one's medical wishes are adhered to, the DNR order is a fundamental piece of ethical medical and personal decision-making.