Fillable Do Not Resuscitate Order Document for New York
When it comes to making decisions about end-of-life care, one document stands out for its critical role in directing healthcare providers on the wishes of the patient—the New York Do Not Resuscitate (DNR) Order form. This legal document, crafted carefully to respect the autonomy and choices of individuals, communicates a person's wish not to have cardiopulmonary resuscitation (CPR) if their heart stops or if they stop breathing. It's a decision that many individuals in New York take seriously, often as part of broader advance care planning. The DNR Order is not just a form; it is a declaration made after careful thought, generally in consultation with healthcare professionals, and in many cases, with close family members or legal representatives involved in the process. It represents a nuanced aspect of healthcare that respects patients' wishes, ensuring that they receive only the types of medical interventions they are comfortable with, especially in life's final moments. Detailed in nature, the form contains specific directions for healthcare professionals, ensuring that there is no ambiguity regarding the patient's wishes, thus safeguarding both the emotional and physical well-being of the patient and their loved ones during incredibly challenging times.
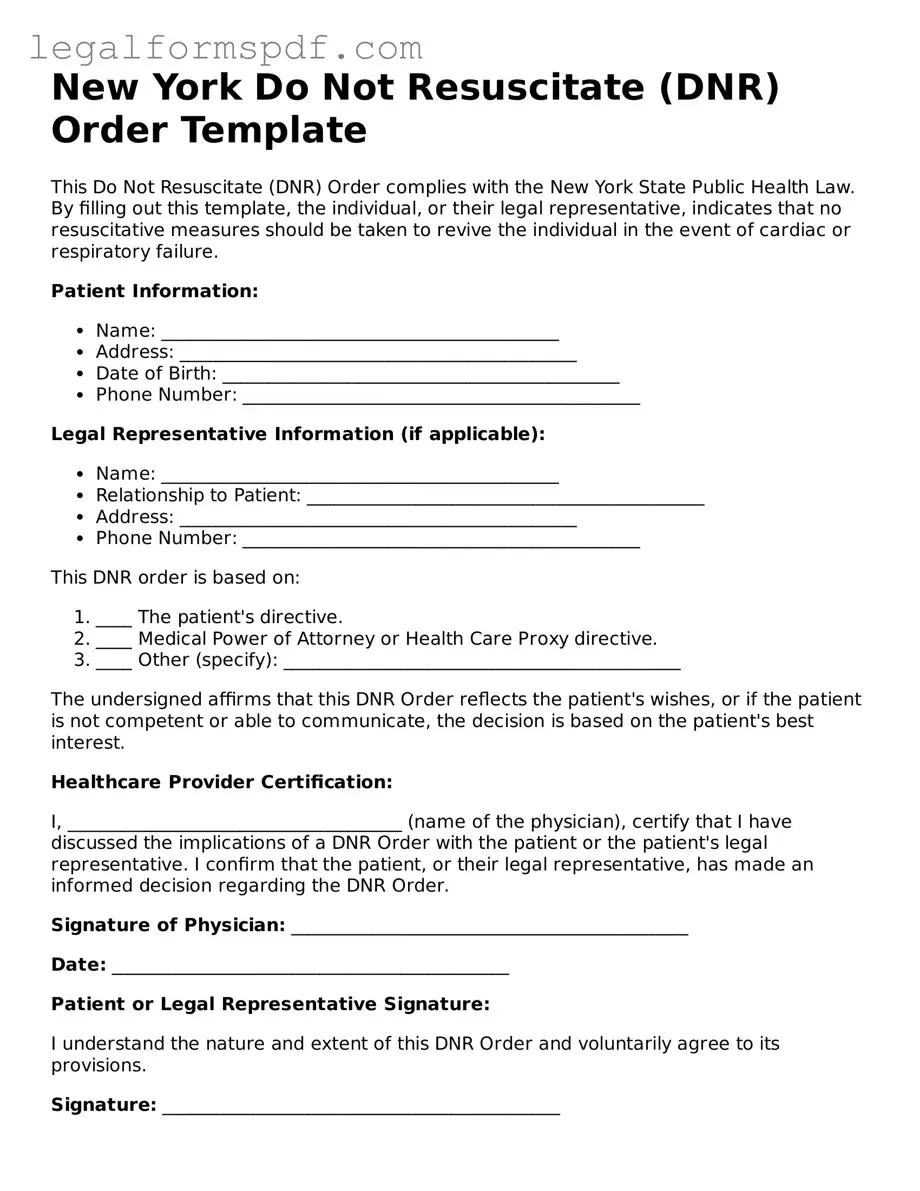
Document Example
New York Do Not Resuscitate (DNR) Order Template
This Do Not Resuscitate (DNR) Order complies with the New York State Public Health Law. By filling out this template, the individual, or their legal representative, indicates that no resuscitative measures should be taken to revive the individual in the event of cardiac or respiratory failure.
Patient Information:
- Name: ____________________________________________
- Address: ____________________________________________
- Date of Birth: ____________________________________________
- Phone Number: ____________________________________________
Legal Representative Information (if applicable):
- Name: ____________________________________________
- Relationship to Patient: ____________________________________________
- Address: ____________________________________________
- Phone Number: ____________________________________________
This DNR order is based on:
- ____ The patient's directive.
- ____ Medical Power of Attorney or Health Care Proxy directive.
- ____ Other (specify): ____________________________________________
The undersigned affirms that this DNR Order reflects the patient's wishes, or if the patient is not competent or able to communicate, the decision is based on the patient's best interest.
Healthcare Provider Certification:
I, _____________________________________ (name of the physician), certify that I have discussed the implications of a DNR Order with the patient or the patient's legal representative. I confirm that the patient, or their legal representative, has made an informed decision regarding the DNR Order.
Signature of Physician: ____________________________________________
Date: ____________________________________________
Patient or Legal Representative Signature:
I understand the nature and extent of this DNR Order and voluntarily agree to its provisions.
Signature: ____________________________________________
Date: ____________________________________________
This DNR Order remains valid unless revoked. To revoke, the patient or their legal representative must inform the attending physician or healthcare provider in writing.
PDF Specifications
| Fact Name | Description |
|---|---|
| Purpose | The New York Do Not Resuscitate (DNR) Order form is used to document an individual's wish not to receive cardiopulmonary resuscitation (CPR) in case their breathing stops or their heart stops beating. |
| Governing Law | In New York, the DNR Order form is governed by Article 29-B of the Public Health Law. |
| Who Can Consent | Consent for a DNR Order can be given by the patient themselves, a health care agent appointed through a Health Care Proxy, a parent or legal guardian (if the patient is a minor or incapacitated), or a surrogate decision-maker under the Family Health Care Decisions Act. |
| Form Requirement | The DNR Order must be documented on a form that is prescribed by the Commissioner of Health or documented in the patient's medical record according to the regulations. |
| Revocation Process | A DNR Order can be revoked at any time by the patient, or their legal representative, by expressing the intent to revoke verbally or in writing to the attending physician or healthcare staff. |
Instructions on Writing New York Do Not Resuscitate Order
Filling out a New York Do Not Resuscitate (DNR) Order form is a critical step for individuals wishing to specify their desires regarding resuscitation in the event they are unable to make such decisions themselves. This form ensures that the patient's wishes are respected by healthcare providers. Below you'll find a detailed guide to accurately completing this form, which must be followed with precision. Once the form is filled out, it is essential that it's placed in a prominent location where emergency personnel can easily find it, and consider providing copies to family members, your healthcare proxy, and your primary care physician.
- Identify the patient: Start by clearly printing the patient's full legal name, address, and date of birth at the top of the form.
- Specify the patient’s wishes: Indicate clearly that the patient does not wish to be resuscitated by checking or marking the appropriate box.
- Healthcare proxy or power of attorney: If applicable, include the name and contact information of anyone holding healthcare proxy or durable power of attorney for healthcare decisions.
- Physician’s information: Fill in the name, address, and contact number of the patient's attending physician. This physician will sign the form, affirming the patient’s DNR status.
- Signature of patient or guardian: If the patient is conscious and able to sign, they should do so in the designated space. If the patient is unable, a legal guardian, healthcare proxy, or family member authorized to make healthcare decisions must sign on their behalf.
- Physician’s signature: The physician must sign the form, confirming the patient’s DNR order. The date of the physician’s signature is also required.
- Witness signature: A witness, who understands the patient's wishes and affirms the authenticity of the patient or guardian's signature, must also sign. Their printed name and the date of their signature are required.
After completing these steps, review the form carefully to ensure all information is accurate and all necessary signatures are in place. It is advisable to discuss these wishes and provide a copy of the signed form to all involved in the care of the individual, including family members and other healthcare providers. Remember, this form can be updated or revoked by the patient at any time, as long as they are mentally competent to do so. Keeping the communication lines open with healthcare providers and loved ones about these decisions is paramount.
Understanding New York Do Not Resuscitate Order
What is a Do Not Resuscitate Order (DNR) in New York?
A Do Not Resuscitate Order, commonly known as a DNR, is a medical order written by a doctor. It instructs health care providers not to perform cardiopulmonary resuscitation (CPR) if a patient's breathing stops or if the patient's heart stops beating. In New York, this order is used to respect the patient's wishes regarding end-of-life care.
How can someone get a DNR order in New York?
To get a DNR order in New York, a patient or their legally authorized representative needs to have a discussion with the patient's doctor. The doctor will explain what the DNR order means, including its benefits and risks. If the patient decides not to receive CPR, the doctor will document this choice in the patient's medical record and will complete the DNR form.
Can a DNR order be revoked or changed once it's in place?
Yes, a DNR order can be revoked or changed at any time by the patient or their legally authorized representative. This can be done by informing the doctor of the wish to revoke the DNR order. The doctor will then document the revocation in the patient's medical record and ensure that the DNR order is no longer in effect.
Is a DNR order the same as an advance directive or living will?
No, a DNR order is not the same as an advance directive or living will. While all these documents relate to a patient's wishes for their medical care, a DNR specifically addresses the use of CPR in emergency situations. Advance directives and living wills, on the other hand, can include a wider range of healthcare preferences and instructions for various medical treatments or conditions.
Who should consider having a DNR order?
People with serious illnesses or at the end of their life who want to avoid aggressive measures such as CPR should consider discussing a DNR order with their doctor. It is also suitable for individuals with specific wishes about their end-of-life care due to religious beliefs, personal preferences, or other reasons.
What happens if a patient is unable to communicate and doesn't have a DNR order in place?
If a patient is unable to communicate their wishes regarding resuscitation and does not have a DNR order in place, healthcare providers will generally attempt resuscitation in case of cardiac or respiratory arrest. This is why it’s important for individuals to discuss their wishes with their family and healthcare providers in advance, to ensure their preferences are known and can be respected.
Common mistakes
Filling out the New York Do Not Resuscitate (DNR) Order form is a significant step that requires attention to detail and a clear understanding of the intentions behind it. One common mistake people make is not discussing their wishes with their family or healthcare provider before completing the form. This lack of communication can lead to conflicts or confusion later on, particularly in emergency situations where loved ones and medical personnel need to understand the individual's preferences quickly and clearly.
Another error involves incorrect or incomplete information. The DNR form requires specific data, including personal identification details and precise medical orders. If any of this information is missing or filled out incorrectly, it might invalidate the form or cause delays when the document needs to be referenced urgently. It is crucial that all information is double-checked for accuracy and completeness.
Many individuals also fail to keep the DNR order accessible. Once the form is completed, it should be kept in a place where it can be easily found by family members or medical responders in an emergency. An inaccessible DNR form is as good as not having one, as it cannot be acted upon if it cannot be found in time.
A further mistake is not updating the DNR order. Life circumstances and health conditions change, which may lead to a change in one's wishes regarding resuscitation. Not revising the DNR order to reflect current wishes can result in medical intervention that is not in line with the individual's current preferences. It is advisable to review and, if necessary, update the document regularly, especially after any significant changes in health status.
Some people mistakenly believe that filling out a DNR form is all that's required for all end-of-life decisions, not realizing it covers specifically the decision not to attempt cardiopulmonary resuscitation (CPR). They might not complete other essential healthcare directives that cover different aspects of end-of-life care, leaving significant gaps in their planning. To ensure wishes are fully respected, completing additional health care directives alongside the DNR order is often necessary.
Lastly, the failure to notify or distribute copies of the DNR order to key individuals is a significant oversight. After the form is correctly filled out, copies should be given to the person’s healthcare provider, local hospital, and any healthcare proxy or family members who may be involved in making medical decisions. Without proper distribution, those who need to be aware of the DNR order may not know of its existence or be able to act on it during critical moments.
Documents used along the form
When preparing for healthcare decisions, especially those concerning end-of-life care, it's crucial to be aware of various documents that complement the New York Do Not Resuscitate (DNR) Order form. These documents are designed to ensure that one's healthcare wishes are known and can be legally respected. They range from specifying types of medical care you wish to receive to appointing someone to make decisions on your behalf. Understanding each document's purpose will help in creating a thorough and coherent healthcare plan.
- Health Care Proxy: This document allows a person to appoint someone they trust (a proxy) to make health care decisions on their behalf if they become unable to make those decisions themselves.
- Living Will: This written, legal document spells out the types of medical treatments and life-sustaining measures a person wants or does not want, such as mechanical ventilation or feeding tubes, if they're unable to communicate their wishes directly.
- Medical Orders for Life-Sustaining Treatment (MOLST): This is a bright pink form designed to communicate a person’s wishes regarding lifesaving treatments, including resuscitation, intubation, and use of ventilators. It's intended for patients with serious health conditions.
- Nonhospital DNR Order: Specific to New York, this form tells emergency medical personnel not to perform CPR on the patient if their heart stops or if they stop breathing. It's applicable in nonhospital settings, like at home.
- Power of Attorney: A legal document giving one person (the agent) the power to conduct legal and financial affairs on another person's (the principal’s) behalf. This can include decisions about paying bills, investing money, or selling property.
- Emergency Medical Information Form: This form provides essential health information, such as allergies, medications, and conditions, to first responders during an emergency where the patient might be unable to communicate.
- HIPAA Release Form: This form permits healthcare providers to share a patient’s medical information with specified individuals, usually family members or other close contacts. It's crucial for ensuring loved ones can stay informed about the patient’s health condition.
- Five Wishes: Often considered a comprehensive living will, this document lets individuals specify their personal, spiritual, and medical wishes in the event they become unable to communicate. It covers aspects like how comfortable they want to be, how they want people to treat them, and what they want their loved ones to know.
Comprehensive planning for healthcare decisions involves more than just a New York DNR Order. These documents collectively ensure that a person’s health care preferences are honored in various situations, offering peace of mind to both the individual and their loved ones. By understanding and completing these forms, individuals can ensure that their healthcare wishes are clearly documented and legally protected.
Similar forms
A Living Will is remarkably similar to the New York Do Not Resuscitate (DNR) Order form, sharing its focus on a person's preferences regarding medical treatment at the end of life. While a DNR specifically instructs healthcare providers not to initiate CPR if a person's heart stops, a Living Will can cover a broader range of medical interventions that the individual wishes to decline or accept, including mechanical ventilation, feeding tubes, and other life-sustaining treatments. Both documents are proactive measures that communicate a patient's healthcare preferences to ensure they are respected.
The Medical Power of Attorney (Healthcare Proxy) document is another one that bears resemblance to the DNR Order form. It designates an agent to make healthcare decisions on behalf of the individual if they become incapable of making those decisions themselves. Similar to a DNR, which clearly states the individual's choice about not receiving CPR, a Medical Power of Attorney outlines the individual's preferences for medical treatment, ensuring decisions are made according to their wishes. Both tools are essential in advance care planning.
The POLST form (Physician Orders for Life-Sustaining Treatment) also shares similarities with the New York DNR Order form. Both are medical orders that take effect immediately and reflect a patient's preferences about the types of life-sustaining treatment they wish to receive or avoid. While the DNR specifically addresses CPR, the POLST form can include instructions on a wider array of treatments, such as antibiotics, intubation, and feeding tubes. Both documents are designed to ensure that healthcare providers are aware of and honor the patient's wishes.
Advance Healthcare Directives closely resemble the DNR Order form, combining elements of both the Living Will and Medical Power of Attorney. These directives provide comprehensive instructions on how an individual's medical care should be handled if they're unable to communicate their decisions. Similar to a DNR, which explicitly refuses CPR, Advance Healthcare Directives can outline a variety of medical treatments the individual does or does not want, including the conditions under which they would prefer to decline life-sustaining measures.
An Organ Donor Card also shares a connection with the DNR Order form, as both deal with decisions made in anticipation of death. While the DNR order specifies not to receive CPR in the event of a cardiac arrest, an Organ Donor Card indicates an individual's choice to donate their organs and tissues after death. Both documents are pivotal in respecting a person's healthcare and posthumous wishes, informing medical personnel and loved ones of their decisions in critical moments.
The Five Wishes Document is another example that parallels the New York DNR Order form. It's an advance directive that goes beyond medical issues, addressing personal, emotional, and spiritual needs alongside medical wishes. Like a DNR, which directs healthcare providers about CPR, Five Wishes allows individuals to document their preferences regarding pain management, living arrangements, their desired comfort level, and how they wish to be treated by others. Both documents empower patients to make their end-of-life preferences known, ensuring they're treated with dignity and respect.
Dos and Don'ts
The New York Do Not Resuscitate (DNR) Order form is a critical document for those who wish to communicate their wishes regarding life-sustaining treatments. Proper completion of this form is essential to ensure that those wishes are respected. Here are some guidelines to help individuals, and their families navigate the process effectively.
Things You Should Do:
- Consult with a healthcare provider to fully understand the implications of a DNR order and how it fits within your overall healthcare plan.
- Ensure all information is legible and accurate to avoid any misunderstandings during emergency situations.
- Discuss your decision with close family members or loved ones to ensure they understand your wishes and the reasoning behind them.
- Sign and date the form as required to make it legally binding. Ensure that the healthcare provider also signs and dates the form.
- Keep the original document in a readily accessible location and provide copies to key family members or caregivers.
- Inform your primary care doctor about your DNR order so it can be included in your medical records.
- Review and update your DNR order as needed, especially if your health condition or preferences change.
- Consider wearing a medical alert bracelet that indicates you have a DNR order, making this information immediately available to healthcare providers in an emergency.
Things You Shouldn't Do:
- Fill out the form without having a thorough discussion with a healthcare professional about what a DNR order means.
- Leave sections of the form blank, as incomplete forms may not be honored in an emergency.
- Fail to communicate your decision to implement a DNR order with key family members and healthcare providers.
- Forget to ensure the DNR order is properly signed and dated, as an unsigned form is not legally valid.
- Overlook the need to keep the form in an accessible place where emergency personnel can easily find it.
- Assume all doctors and hospitals have access to your DNR order without providing them with a copy.
- Refuse to reconsider your DNR status if your health situation significantly changes.
- Rely solely on verbal instructions without completing the formal DNR documentation process.
Misconceptions
Understanding the New York Do Not Resuscitate (DNR) Order can sometimes be complicated due to prevailing misconceptions. This document aims to clarify these misconceptions, offering accurate information to ensure that individuals are fully informed about what a DNR Order entails.
A DNR Order is only for the elderly: Contrary to common belief, a DNR Order can apply to anyone at any age whose medical condition suggests that resuscitation would not benefit their quality of life or align with their healthcare wishes.
Signing a DNR means giving up on all types of medical treatments: This is incorrect. A DNR specifically refers to not performing cardiopulmonary resuscitation (CPR) in the event of cardiac or respiratory arrest. It does not impact other treatments or interventions a patient may receive.
Doctors decide to issue DNR Orders without consulting the patient or family: In New York, a DNR Order is only placed after thorough discussion with the patient (if possible) or the patient’s healthcare proxy or family. The patient’s wishes are paramount in this decision-making process.
A DNR Order can only be revoked by a doctor: Patients or their designated healthcare proxies have the right to revoke a DNR Order at any time. It is crucial that this wish is communicated clearly to the healthcare team.
Having a DNR means you cannot be admitted to a hospital: This is a misconception. A DNR Order does not limit access to hospital care. It only instructs healthcare providers not to initiate CPR in the event of cardiac or respiratory failure.
Emergency services will not assist someone with a DNR: Emergency medical personnel will provide all necessary care, except for CPR, to a patient with a DNR Order. They are trained to offer comprehensive medical attention while respecting the DNR stipulations.
A DNR Order is the same as a Living Will: Though both are advance directives, they serve different purposes. A DNR specifically addresses CPR in an emergency, whereas a Living Will covers a broader range of medical interventions and treatments at the end of life.
A DNR must be posted in the home to be valid: While it's important for a DNR Order to be readily accessible in the event of an emergency, there is no legal requirement in New York that it must be posted in one's home. However, it should be easily available to show to emergency personnel.
Once a DNR Order is signed, it cannot be changed: DNR Orders can be updated or revoked at any time to reflect changes in the patient's health condition or preferences. Communication with healthcare providers is key to ensure that the DNR accurately represents the patient's current wishes.
Dispelling these misconceptions about the New York Do Not Resuscitate Order is crucial for making informed healthcare decisions. Individuals are encouraged to discuss their wishes and concerns with their healthcare providers to ensure that their healthcare preferences are understood and respected.
Key takeaways
Understanding the New York Do Not Resuscitate (DNR) Order form is crucial for making informed decisions about end-of-life care. Here are key takeaways to guide you through filling out and using the form:
- Know the Purpose: A DNR order informs healthcare providers not to perform cardiopulmonary resuscitation (CPR) if a person's breathing or heart stops.
- Consult with a Healthcare Provider: Before completing the form, have a thorough discussion with a healthcare provider to fully understand the implications and ensure it aligns with the person's wishes.
- Form Must Be Signed: The DNR form requires signatures from the person or their healthcare proxy/legally authorized representative, and a physician, nurse practitioner, or physician assistant to be valid.
- Clear Identification: Ensure the person's full name and other identifying information are clearly printed on the form to avoid any confusion.
- Keep It Accessible: Once signed, the DNR order should be kept in a place where it can be easily found by family members and healthcare providers, such as with other important documents or on the refrigerator.
- Review Periodically: Circumstances and wishes can change; therefore, it's important to review and potentially update the DNR order periodically with a healthcare provider.
- Inform Family and Caregivers: Make sure family members and caregivers are aware of the DNR order and understand its significance to ensure the person's wishes are followed.
- It Can Be Revoked: A person can revoke their DNR order at any time by informing their healthcare provider either verbally or in writing.
Approaching the subject of a DNR order can be challenging, but having a clear and valid DNR form is a vital step in respecting the healthcare wishes of individuals at the end of life.
More Do Not Resuscitate Order State Forms
Il Polst Form - The document can serve as a tool for advocacy, empowering patients and their families to assert control over medical treatment decisions.
Dnr Directive - Legal document preventing life-saving measures in the event of cardiac or respiratory arrest.