Fillable Do Not Resuscitate Order Document for Michigan
Understanding the Michigan Do Not Resuscitate Order form is essential for residents who wish to make informed decisions about their end-of-life care. This document plays a pivotal role in medical and emergency situations, where it informs healthcare professionals of a patient's desire to forgo resuscitation attempts in the event their heart stops or they stop breathing. Given its significance, it's crucial to be knowledgeable about how to properly complete and maintain the form, the legal implications it carries, and the circumstances under which it becomes effective. The form also requires the signatures of the individual (or their authorized representative) and a witness, ensuring that the decision is well-documented and legitimate. For individuals looking to respect their loved ones' wishes or make their own choices known, understanding the Michigan Do Not Resuscitate Order form is the first step towards ensuring their directives are followed, thus granting peace of mind to all involved.
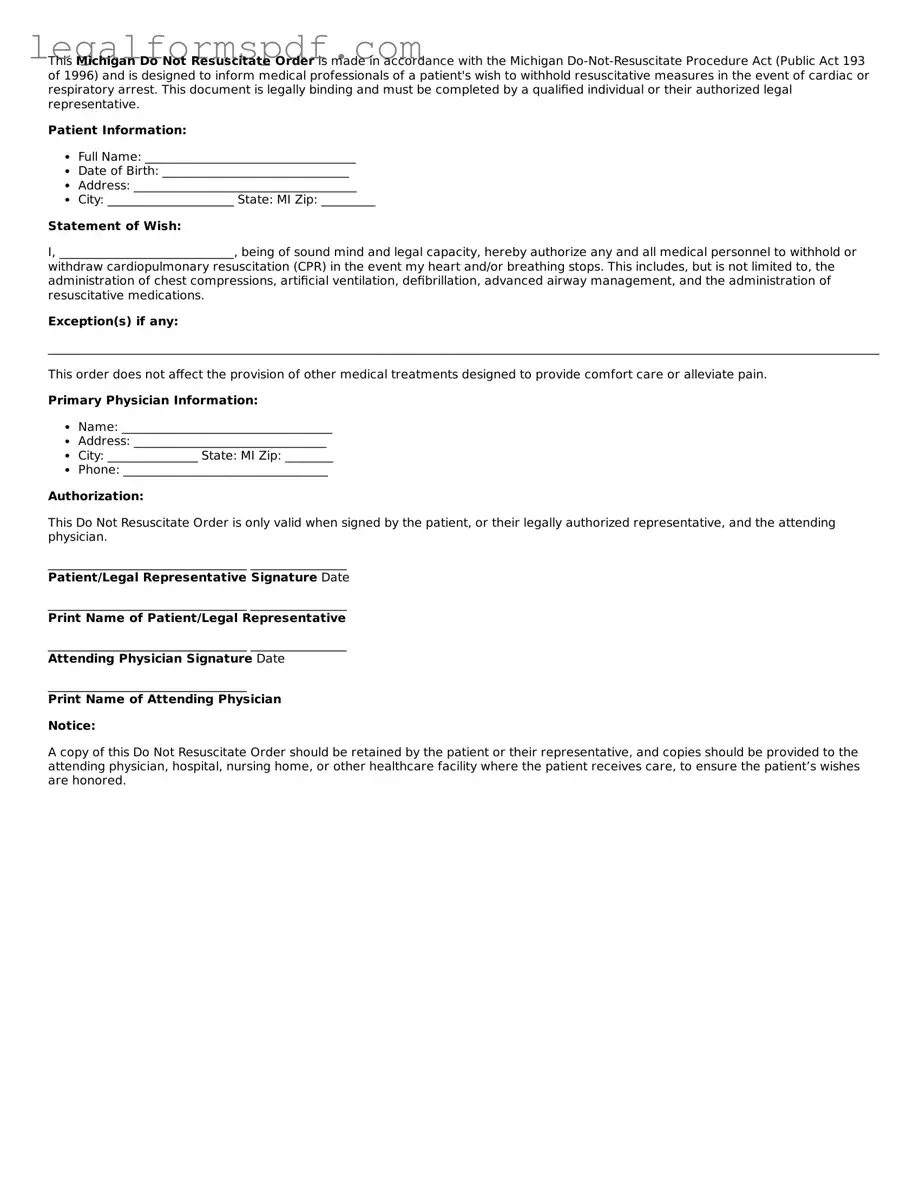
Document Example
This Michigan Do Not Resuscitate Order is made in accordance with the Michigan Do-Not-Resuscitate Procedure Act (Public Act 193 of 1996) and is designed to inform medical professionals of a patient's wish to withhold resuscitative measures in the event of cardiac or respiratory arrest. This document is legally binding and must be completed by a qualified individual or their authorized legal representative.
Patient Information:
- Full Name: ___________________________________
- Date of Birth: _______________________________
- Address: _____________________________________
- City: _____________________ State: MI Zip: _________
Statement of Wish:
I, _____________________________, being of sound mind and legal capacity, hereby authorize any and all medical personnel to withhold or withdraw cardiopulmonary resuscitation (CPR) in the event my heart and/or breathing stops. This includes, but is not limited to, the administration of chest compressions, artificial ventilation, defibrillation, advanced airway management, and the administration of resuscitative medications.
Exception(s) if any:
________________________________________________________________________________________________________________________________________________________
This order does not affect the provision of other medical treatments designed to provide comfort care or alleviate pain.
Primary Physician Information:- Name: ___________________________________
- Address: ________________________________
- City: _______________ State: MI Zip: ________
- Phone: __________________________________
Authorization:
This Do Not Resuscitate Order is only valid when signed by the patient, or their legally authorized representative, and the attending physician.
_________________________________ ________________
Patient/Legal Representative Signature Date
_________________________________ ________________
Print Name of Patient/Legal Representative
_________________________________ ________________
Attending Physician Signature Date
_________________________________
Print Name of Attending Physician
Notice:
A copy of this Do Not Resuscitate Order should be retained by the patient or their representative, and copies should be provided to the attending physician, hospital, nursing home, or other healthcare facility where the patient receives care, to ensure the patient’s wishes are honored.
PDF Specifications
| Fact | Detail |
|---|---|
| Purpose | Allows individuals in Michigan to refuse CPR in case their breathing stops or heart stops beating. |
| Governing Law | Michigan Do-Not-Resuscitate Procedure Act, Public Act 193 of 1996 |
| Who Can Sign | The order must be signed by the patient, or their legal guardian or patient advocate if the patient is unable to do so. |
| Witness Requirement | Two witnesses must observe the signing of the Do Not Resuscitate (DNR) Order. |
| Form Validity | The form is valid across Michigan but should be considered portable and kept with the individual. |
| Revocation Process | The DNR order can be revoked verbally or in writing by the patient, or by a clear indication of the patient's intent to receive resuscitation. |
Instructions on Writing Michigan Do Not Resuscitate Order
When someone in Michigan decides not to receive CPR (cardiopulmonary resuscitation) if their heart stops or they stop breathing, they use a Do Not Resuscitate (DNR) Order form. This document ensures their wishes are respected by healthcare providers. Completing this form can seem overwhelming, but breaking it down into steps makes it more manageable. It's a vital step for ensuring one's end-of-life care preferences are understood and honored.
To fill out the Michigan Do Not Resuscitate Order form, follow these steps:
- Gather personal information, including the full legal name, address, and date of birth of the person the DNR order is for.
- Read through the entire form to understand the nature and implications of a Do Not Resuscitate Order.
- Complete the section of the form that requires the personal information mentioned in step 1.
- If the individual is competent to make their own healthcare decisions, they should sign and date the form in the designated area.
- In cases where the individual is not capable of signing for themselves, a legally authorized representative (such as a healthcare proxy, power of attorney for healthcare, or next of kin) may sign on their behalf. Ensure the representative's full name, relationship to the individual, and contact information are clearly written.
- The attending physician must also sign and date the form, confirming their discussion with the individual or their representative about the decision not to seek CPR in cases of cardiac or respiratory arrest.
- Keep the completed form in an easily accessible location and inform family members, caregivers, and healthcare providers of its existence and location.
After completing the DNR form, it's essential to remember that it can be revoked at any time by the individual it covers, or their legally authorized representative, if the individual's decision-making capacity has been compromised. To revoke a DNR, it's advised to inform the attending physician verbally or in writing. Keeping all parties informed ensures that the individual’s current wishes about end-of-life care are known and respected.
Understanding Michigan Do Not Resuscitate Order
What is a Do Not Resuscitate (DNR) Order in Michigan?
A Do Not Resuscitate (DNR) Order in Michigan is a legal document that tells medical personnel not to perform CPR if a person's breathing stops or if the heart stops beating. It is used by individuals who want to decline life-sustaining treatments in those specific circumstances.
Who can request a DNR Order in Michigan?
Any competent adult can request a DNR Order in Michigan. This includes individuals who, after being fully informed of the nature and consequence of a DNR Order, decide that they do not want to receive CPR in the event of cardiac or respiratory arrest. Additionally, legal guardians or agents with durable power of attorney for healthcare decisions can request a DNR on behalf of someone else.
How can one obtain a DNR Order in Michigan?
Obtaining a DNR Order in Michigan involves consulting with a healthcare provider. The healthcare provider can help understand the implications of a DNR Order and assist with the appropriate forms. Once the DNR form is completed and signed by the appropriate parties, including the individual or their legal representative and the physician, it becomes valid.
Is the Do Not Resuscitate Order valid in all settings in Michigan?
The Michigan DNR Order is recognized in various settings, including hospitals, homes, and hospice care. However, its enforcement can vary depending on the setting and the specific circumstances. For instance, in a hospital, the DNR Order should be included in the patient's medical record to ensure it is respected by the medical staff.
What happens if medical personnel are not aware of a DNR Order?
If medical personnel are unaware of an existing DNR Order, they are likely to proceed with all available life-saving measures, including CPR. It is crucial for patients or their representatives to inform medical staff about the DNR Order and to provide documentation if available.
Can a DNR Order be revoked or changed in Michigan?
Yes, a DNR Order in Michigan can be revoked or changed at any time by the individual who issued it or their legal representative. This can be done by informing the healthcare provider verbally or in writing. Following a revocation, a new DNR Order will need to be completed and signed if the individual decides to reinstate it.
Does having a DNR Order affect the quality of other treatments in Michigan?
No. A DNR Order specifically addresses the use of CPR in cases of cardiac or respiratory arrest. It does not impact the right to receive other types of medical treatments or interventions. Healthcare providers will continue to offer all other indicated treatments and palliative care to ensure comfort and quality of life.
What legal protection does the person signing the DNR Order have in Michigan?
In Michigan, individuals who have signed a DNR Order, their families, and healthcare providers acting in accordance with an acknowledged DNR Order are protected under state law. This means they cannot be held legally responsible for the natural consequences of withholding CPR as directed by the DNR Order.
Where should a DNR Order be kept to ensure it is respected in Michigan?
A DNR Order should be kept in an easily accessible place where it can be quickly shown to emergency personnel or healthcare providers. Many individuals choose to keep a copy at home in clear view and also inform family members, caregivers, and/or their legal representative of its location. When outside the home or in other care settings, carrying a copy or wearing a DNR bracelet can help communicate the individual's wishes effectively.
Common mistakes
Filling out the Michigan Do Not Resuscitate (DNR) Order form can be a challenging process, fraught with emotional decisions and the requirement for precision. A significant mistake often made is neglecting to clearly understand the implications of a DNR order. Individuals, at times, without fully grasping what it entails, may choose this option under stressful conditions. DNR orders are crucial medical directives that should be considered with full awareness of their meanings, implications, and consequences, ensuring decisions align with the person's wishes.
Another common error involves inaccuracies or incomplete sections on the form. Every field in the DNR form serves a specific purpose, outlining patient information, medical conditions, and the orders themselves. Mistakes or omissions can lead to ambiguity, potentially resulting in medical professionals being unable to honor the DNR directive. Accuracy is paramount, as is ensuring no section is left unfilled, to convey clear instructions for healthcare providers.
Many individuals also miss the crucial step of obtaining the necessary signatures to validate the form. A Michigan DNR order requires the signature of the individual (or their authorized representative) and a witness, as well as the attending physician. Without these endorsements, the document may not be legally recognized, undermining its purpose and the individual's wishes in critical moments. This oversight can easily void the document, leading to unwanted medical interventions.
A fourth mistake is failing to discuss the decision with family members and healthcare providers. Communication is key in these matters. When family members are unaware of the DNR order or the reasoning behind it, it can lead to conflicts or confusion during emergencies. Similarly, if healthcare providers are not informed of the DNR order in advance, they may not act in accordance with the individual's wishes. These discussions, though potentially difficult, are essential for ensuring that everyone involved understands and respects the person's healthcare decisions.
Last but not least, not regularly reviewing and updating the DNR order constitutes a critical oversight. Personal wishes and health conditions can change over time, necessitating revisions to previously made decisions. A DNR order made years ago may no longer reflect an individual's current wishes. Regular reviews and, if necessary, updates to the DNR order ensure it accurately represents the individual's preferences, providing peace of mind to all involved.
Documents used along the form
When dealing with health and end-of-life decisions, the Michigan Do Not Resuscitate (DNR) Order form is a significant document that stipulates a person's wishes not to have CPR (Cardiopulmonary Resuscitation) in the event their heart stops or they stop breathing. However, this document often works in tandem with several other forms to ensure a comprehensive approach to an individual’s healthcare wishes. These documents can provide additional instructions and specify other preferences regarding an individual's medical care and treatment. Understanding these forms is crucial for making informed decisions that align with one’s values and wishes.
- Living Will: This document complements the DNR order by providing detailed instructions on a wide range of life-sustaining treatments beyond CPR, in case the individual becomes unable to communicate their healthcare preferences. It allows individuals to specify their wishes regarding artificial hydration, ventilation, and other forms of medical intervention.
- Medical Power of Attorney (Healthcare Proxy): This document appoints a trusted person to make healthcare decisions on behalf of the individual, should they become incapacitated and unable to make decisions for themselves. The designated person has the authority to consult with healthcare providers and make decisions that align with the individual's previously expressed wishes, which can include adhering to the DNR order.
- POLST (Physician Orders for Life-Sustaining Treatment) Form: Unlike the DNR order, which is specifically about CPR, the POLST form provides broader orders regarding other types of life-sustaining treatments (like feeding tubes or antibiotics) based on the individual's current health condition. This form is intended for seriously ill or frail patients and is filled out after a detailed conversation with their physician or healthcare provider.
- Advance Directive: Sometimes used interchangeably with a Living Will, an Advance Directive allows individuals to document their preferences for end-of-life care, including resuscitation. It can also encompass a Medical Power of Attorney, making it a comprehensive document that addresses various aspects of healthcare decision-making and personal values regarding treatment.
Understanding and completing these documents can seem daunting. However, they are essential tools for ensuring that an individual’s healthcare preferences are known, respected, and followed. Healthcare professionals strongly encourage having conversations about these documents with family members and healthcare providers early on, not just when facing a medical crisis. Together, they form a critical foundation for personal autonomy and peace of mind, knowing that one’s healthcare wishes will be honored.
Similar forms
The Michigan Do Not Resuscitate (DNR) Order shares similarities with an Advance Directive, as both documents cater to an individual's healthcare preferences at times when they can't express their wishes. Like a DNR, an Advance Directive may include stipulations on whether to administer life-extending treatments or not. However, an Advance Directive is broader, potentially encompassing preferences about organ donation and designating a healthcare proxy.
A Living Will, often part of an Advance Directive, is also closely related to a DNR. It specifically instructs healthcare providers regarding the types of life-sustaining treatments an individual wishes to decline in the event they become terminally ill or permanently unconscious. A Living Will is more comprehensive, addressing a wider array of medical interventions than a DNR, which is solely focused on not initiating resuscitation attempts.
Power of Attorney for Healthcare is akin to a DNR in that it pertains to medical decisions made when one is incapacitated. This document appoints a healthcare agent to make decisions on the individual's behalf, which could include enforcing or not enforcing DNR orders. Unlike a DNR, which is a direct instruction, a Power of Attorney for Healthcare delegates decision-making power to another.
The HIPAA Release Form, while primarily focused on privacy and the sharing of medical information, intersects with the DNR's domain through the facilitation of informed medical decisions. By allowing designated individuals to access one’s medical records, decisions regarding DNR orders can be made more comprehensively, based on full knowledge of the individual's medical history and current condition.
A POLST (Physician Orders for Life-Sustaining Treatment) form closely mirrors the intent behind a DNR by translating an individual's treatment preferences into medical orders to be followed by healthcare professionals. It differs in its broader application, covering a wide range of end-of-life care decisions beyond CPR, including ventilation, antibiotic use, and artificial nutrition.
The Five Wishes Document goes beyond the clinical aspects covered by a DNR, touching on personal, emotional, and spiritual desires at the end of life. It helps guide medical treatment, like a DNR, but also addresses comfort care, dignity, and how the individual wishes to be treated by others. This holistic approach to end-of-life planning provides a comprehensive framework that encompasses but is not strictly limited to medical intervention choices.
Last, an Organ and Tissue Donation Registration form, while not a directive about the provision or withholding of life-sustaining treatment, is relevant in the context of post-mortem decisions. Like a DNR, it represents a proactive decision about one's body and how it should be treated in the absence of the capacity to communicate one’s wishes, focusing on the possibility of organ donation after death.
Dos and Don'ts
When filling out the Michigan Do Not Resuscitate (DNR) Order form, it's important to approach the task with care and attention. Here are some guidelines to help ensure the process is done correctly and respectfully:
What you should do:
- Read the instructions on the form carefully to ensure you understand all the requirements.
- Include all required personal information accurately to avoid any issues with identification.
- Consult with a healthcare professional if you have any questions about how a DNR order might affect your medical care.
- Make sure the form is signed by the required parties, which usually include the patient or their legal representative and the attending physician.
- Keep a copy of the completed form in an easily accessible place, and inform close family members or caregivers of its existence and location.
- Consider wearing a DNR bracelet or carrying a DNR card as an additional way to communicate your wishes to healthcare providers in an emergency.
What you shouldn't do:
- Do not fill out the form without thoroughly understanding the implications of a DNR order.
- Avoid leaving any sections of the form incomplete, as this could lead to misunderstandings or legal complications.
- Don't sign the form without ensuring that all the information is correct and reflects the wishes of the person it concerns.
- Refrain from keeping the completed form in a place where it is difficult for family members or emergency personnel to find.
- Do not fail to communicate your decision to opt for a DNR order with your family and healthcare providers.
- Avoid assuming that a DNR order is permanent; it can be revoked or modified at any time by the person it pertains to or their legal representative.
Misconceptions
The Michigan Do Not Resuscitate (DNR) Order form is surrounded by misconceptions that often lead to confusion about its purpose and implications. Understanding these misunderstandings is crucial for individuals making informed decisions about their end-of-life care. Here are eight common misconceptions:
- Only the elderly or terminally ill can have a DNR order. In fact, Michigan allows anyone with a serious illness or at significant risk of death in the near future to request a DNR, regardless of their age.
- A DNR order means no medical treatment will be provided. This is not accurate. A DNR specifically addresses the avoidance of resuscitative efforts like CPR if a person's breathing stops or the heart stops beating. It does not mean that other forms of medical care, such as pain relief, cannot be provided.
- Doctors can override a DNR if they disagree with it. Under Michigan law, healthcare providers must respect a valid DNR order. They cannot override it based on personal beliefs or preferences. However, in emergency situations where a valid DNR is not immediately available, resuscitation might inadvertently occur.
- A DNR order is permanent and cannot be changed. Actually, a DNR can be revoked or amended at any time by the individual or their legally authorized representative, as long as they are competent to do so.
- You need a lawyer to complete a DNR order. While legal advice might be beneficial in certain situations, Michigan residents can complete a DNR order form without needing a lawyer. It does need to be signed by a healthcare provider to be valid.
- A DNR applies in all situations. A DNR order is specifically for preventing resuscitation in cases where breathing ceases or the heart stops. It has no bearing on other medical treatments or interventions that may be necessary under different circumstances.
- Hospital DNR orders are the same as out-of-hospital orders. Michigan differentiates between in-hospital and out-of-hospital DNR orders. The requirements and applicability of these orders can vary, so it's important to understand the specific conditions of each.
- Family members can authorize a DNR on behalf of the patient at any time. Consent must come directly from the patient if they are of sound mind to make their own medical decisions or from an individual legally authorized to make decisions on their behalf. Family members cannot unilaterally make this decision without proper legal authorization.
Dispelling these misconceptions is essential for ensuring that individuals are fully informed about the DNR process and its impact on medical care. Anyone considering a DNR should discuss their options and concerns with a healthcare provider to make the decision that best aligns with their wishes and health care goals.
Key takeaways
In Michigan, a Do Not Resuscitate (DNR) Order is a crucial document for those who wish to express their preference not to receive CPR (cardiopulmonary resuscitation) in the event their heart stops or they stop breathing. The following key takeaways provide essential information about filling out and using the Michigan DNR Order form:
- Understanding the Purpose: The DNR Order informs healthcare providers and emergency personnel that a patient does not wish to receive CPR in case of a cardiac or respiratory arrest. This decision is respected across various settings, including hospitals, homes, and public places.
- Eligibility Criteria: Any individual of sound mind and aged 18 or older can request a DNR Order. Minors can also have a DNR Order, but it requires the consent of a parent or guardian.
- Mandatory Consultation: Before completion, the individual, or their legal representative, must consult with a healthcare provider to understand the implications fully and ensure the decision aligns with the patient's health status and personal wishes.
- Form Completion: The Michigan DNR Order form must be thoroughly and accurately completed. It requires essential information, including the patient’s full name, date of birth, and specific medical instructions regarding the DNR order.
- Signing Requirements: The form must be signed by the individual the DNR Order concerns or their legally authorized representative. Additionally, the signature of a physician, nurse practitioner, or physician's assistant is required to validate the order.
- Revocation Process: It is important to note that the individual or their authorized representative can revoke the DNR Order at any time, through any means of communication, whether verbal or written. Healthcare providers should be immediately informed about the revocation.
- Emergency Situations: In emergency situations, paramedics and other first responders will check for a DNR Order, which is often kept in a visible area or worn as a bracelet or necklace by the patient.
- Legal Protection: Healthcare providers and family members are legally protected from liability when they follow a DNR Order in good faith, even in challenging emotional circumstances.
- Copy Distribution: After the DNR Order is signed, it’s vital to distribute copies to relevant individuals, including family members, healthcare proxies, and primary care physicians, to ensure the order is respected and followed.
- Review and Update: The DNR Order should be reviewed periodically, especially after any major change in health status or personal wishes. If necessary, the DNR Order can be updated or revoked to reflect the current desires of the individual.
The Michigan DNR Order is a significant legal document that supports individuals' rights to make informed decisions about their healthcare. Proper completion, distribution, and respect for the DNR Order can ensure that an individual's end-of-life wishes are honored, providing peace of mind for both the individual and their loved ones.
More Do Not Resuscitate Order State Forms
Dnr Form New York - It helps in avoiding the emotional and financial burden on families by aligning medical interventions with the patient's personal values and desires.
Printable Dnr Form - By choosing a DNR Order, patients can make their wishes known, potentially relieving their loved ones from making difficult decisions during emotional times.
Dnr Form Ohio - Helps ensure that medical interventions align with the patient's overall goals of care and quality of life expectations.