Fillable Do Not Resuscitate Order Document for Illinois
Understanding one's options regarding end-of-life care is a crucial aspect of healthcare planning, and for residents of Illinois, the Do Not Resuscitate (DNR) Order form plays a significant role in this process. This form is a legal document that communicates a person's wish not to have cardiopulmonary resuscitation (CPR) performed in the event that their heart stops beating or they stop breathing. The Illinois DNR Order is vital for ensuring that medical and emergency personnel respect the healthcare preferences of individuals during critical moments. It requires thorough consideration and discussion with healthcare providers and family members to ensure that the individual’s wishes are appropriately documented and understood. Not only does the form have implications for the type of medical interventions an individual will receive, but it also influences how emergency services respond in a crisis. It’s an essential tool for anyone looking to have control over their end-of-life care, making its understanding and correct execution paramount.
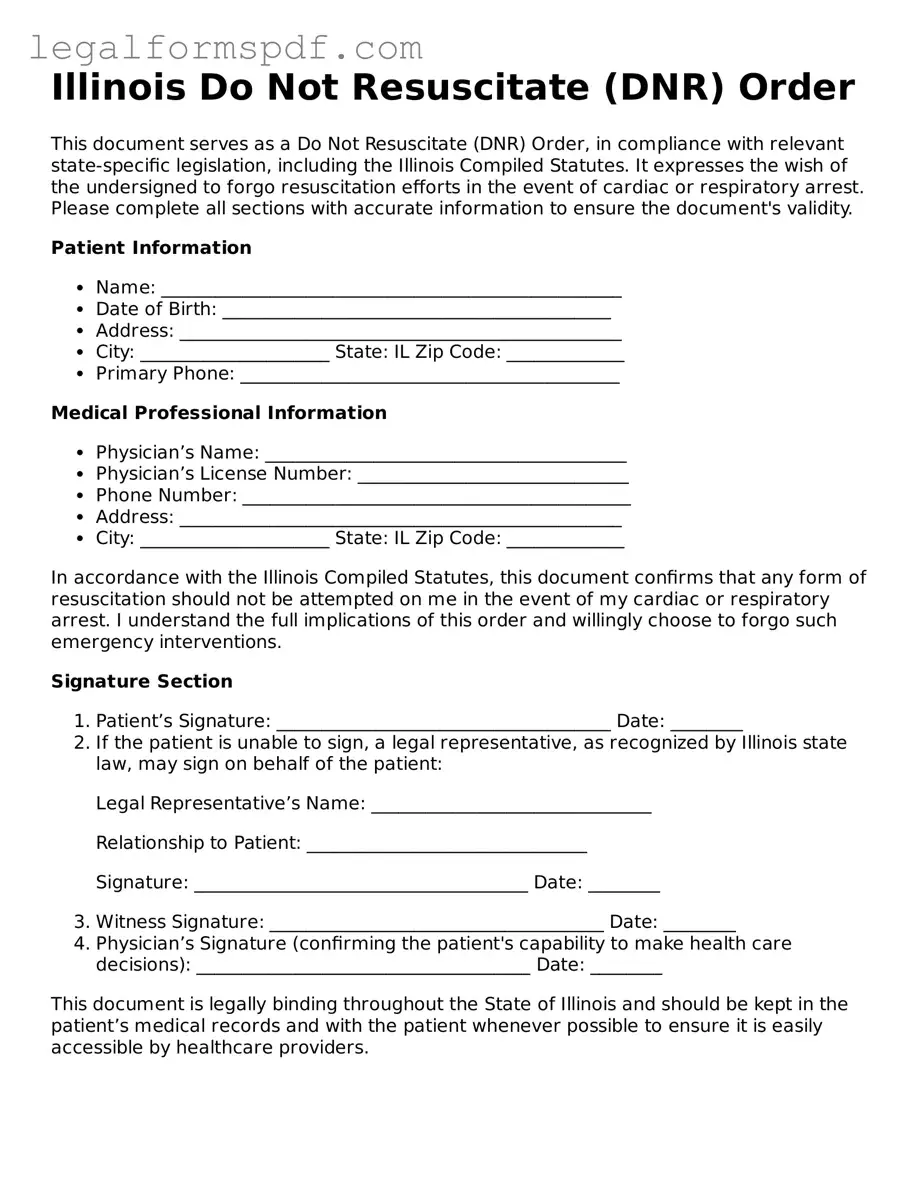
Document Example
Illinois Do Not Resuscitate (DNR) Order
This document serves as a Do Not Resuscitate (DNR) Order, in compliance with relevant state-specific legislation, including the Illinois Compiled Statutes. It expresses the wish of the undersigned to forgo resuscitation efforts in the event of cardiac or respiratory arrest. Please complete all sections with accurate information to ensure the document's validity.
Patient Information
- Name: ___________________________________________________
- Date of Birth: ___________________________________________
- Address: _________________________________________________
- City: _____________________ State: IL Zip Code: _____________
- Primary Phone: __________________________________________
Medical Professional Information
- Physician’s Name: ________________________________________
- Physician’s License Number: ______________________________
- Phone Number: ___________________________________________
- Address: _________________________________________________
- City: _____________________ State: IL Zip Code: _____________
In accordance with the Illinois Compiled Statutes, this document confirms that any form of resuscitation should not be attempted on me in the event of my cardiac or respiratory arrest. I understand the full implications of this order and willingly choose to forgo such emergency interventions.
Signature Section
- Patient’s Signature: _____________________________________ Date: ________
- If the patient is unable to sign, a legal representative, as recognized by Illinois state law, may sign on behalf of the patient:
Legal Representative’s Name: _______________________________
Relationship to Patient: _______________________________
Signature: _____________________________________ Date: ________
- Witness Signature: _____________________________________ Date: ________
- Physician’s Signature (confirming the patient's capability to make health care decisions): _____________________________________ Date: ________
This document is legally binding throughout the State of Illinois and should be kept in the patient’s medical records and with the patient whenever possible to ensure it is easily accessible by healthcare providers.
PDF Specifications
| # | Fact | Description |
|---|---|---|
| 1 | Definition | A Do Not Resuscitate (DNR) Order in Illinois is a legal form that tells medical personnel not to perform CPR if a person's breathing stops or if the heart stops beating. |
| 2 | Governing Law | The Illinois DNR order is governed by the Illinois Compiled Statutes, specifically the Medical Patient Rights Act. |
| 3 | Eligibility | To have a DNR order, an individual must be at least 18 years old, of sound mind, and capable of making their own healthcare decisions, or have a legal guardian or power of attorney who can make these decisions for them. |
| 4 | Physician's Role | A licensed physician must sign the DNR order, indicating that they have discussed the risks and benefits with the patient or the patient's legal representative. |
| 5 | Revocation | The DNR order can be revoked at any time by the patient or their legal representative, either verbally or in writing, without the need for a witness or notarization. |
| 6 | Out of Hospital DNR | Illinois also has an Out of Hospital DNR order specifically for use outside of hospital settings, like in a patient's home, which covers emergency medical services personnel. |
| 7 | Form Requirements | The form must include the patient's name, date of birth, and other identifying information, along with the signature of the patient (or representative) and the physician. |
| 8 | Identification | Patients with a DNR order are often encouraged to wear identifying bracelets or necklaces that notify emergency personnel of their DNR status. |
| 9 | Limitations | The DNR order only applies to CPR and does not affect other treatments, such as pain relief, nutrition, or other potentially life-sustaining measures unless specified in an advance directive. |
| 10 | Public Awareness | Efforts have been made to increase public awareness and understanding of DNR orders in Illinois, including education on the importance of discussing these decisions with family and healthcare providers. |
Instructions on Writing Illinois Do Not Resuscitate Order
In the State of Illinois, individuals have the right to make decisions regarding their healthcare, including the decision not to receive resuscitative efforts in the event of a cardiac or respiratory arrest. This decision is legally recognized through the Illinois Do Not Resuscitate (DNR) Order form, a crucial document for ensuring that one's healthcare preferences are followed. By accurately completing this form, individuals can communicate their wishes clearly to healthcare professionals and loved ones. The following steps provide guidance on how to fill out this important document.
- Begin by reading the entire form to understand its provisions and requirements. It's critical to be fully informed about the implications of a DNR order.
- Enter the patient's full legal name at the top of the form, ensuring it matches the name on their government-issued identification to avoid any confusion.
- Specify the date of birth of the patient to assist healthcare providers in accurately identifying the patient's medical records.
- Fill in the patient's address, including city, state, and zip code, providing a complete picture of the patient's residency for legal and medical purposes.
- Provide the patient's preferred telephone number and an alternative, if available, to ensure reliable communication channels are established.
- Record the name, address, and phone number of the patient’s primary physician. This information is crucial for healthcare providers to consult with the physician who is most familiar with the patient's medical history and care preferences.
- If the patient is signing the DNR order themselves, they must sign and date the form in the designated section. This act formally indicates the patient's decision and understanding of the DNR order's purpose and effect.
- In cases where the patient is unable to sign due to physical incapacity or other reasons, a legally authorized individual may sign on the patient's behalf. This signer must also provide their relationship to the patient and the reason the patient is unable to sign.
- The patient’s physician must also sign and date the form, confirming that the patient is fully aware of the nature and consequences of the DNR order and that it complies with the patient's wishes.
Once completed, the Illinois Do Not Resuscitate Order form must be kept in a location that is easily accessible to first responders and healthcare providers, such as with the patient's other important medical documents or in a visible place within the patient's residence. Additionally, it's advisable to inform close family members, caregivers, and the primary physician of the existence and location of the DNR order to ensure it is respected and implemented according to the patient's wishes.
Understanding Illinois Do Not Resuscitate Order
What is a Do Not Resuscitate (DNR) Order in Illinois?
A Do Not Resuscitate Order in Illinois is a medical directive written by a doctor that informs healthcare providers not to perform cardiopulmonary resuscitation (CPR) if a patient's breathing stops or if the patient's heart stops beating. It is designed for patients with severe illnesses, or those who are at the end of their life, to prevent unnecessary and unwanted medical interventions.
How can someone obtain a DNR Order in Illinois?
To obtain a DNR Order in Illinois, a conversation with a healthcare provider is the first step. The healthcare provider, often a doctor, will discuss the patient's health condition, goals, and values regarding end-of-life care. After this discussion, if a DNR is considered appropriate, the healthcare provider will write the order. It's important that this decision is made by the patient (if able) or by a legally authorized representative if the patient is unable to make medical decisions.
Who should consider a DNR Order?
Individuals with a terminal illness or those with chronic, severe medical conditions who wish to avoid aggressive life-saving measures may consider a DNR Order. It is also suitable for those who value quality of life over extending life through medical interventions. Consulting with a healthcare provider can help in making an informed decision.
Is a DNR Order permanent?
No, a DNR Order is not permanent. It can be revoked or altered at any time by the patient or their designated healthcare proxy. Communication with healthcare professionals is vital to ensure that any changes to the DNR Order are clearly understood and properly documented.
Does having a DNR Order affect the quality of care a patient receives?
No, having a DNR Order does not affect the quality of care provided to a patient. The order specifically relates to CPR and does not limit other types of medical treatments or interventions. Patients with a DNR Order will still receive comprehensive care aimed at comfort, pain relief, and other treatment objectives that align with their wishes and health needs.
Can family members override a DNR Order in Illinois?
Family members cannot override a DNR Order in Illinois if the order reflects the patient's wishes and was appropriately obtained. However, situations may arise where family members disagree with the patient's decision. These cases highlight the importance of clear communication and legal documentation, such as healthcare powers of attorney, to ensure that the patient's desires are honored.
What should be done with the DNR Order once it's obtained?
Once a DNR Order is obtained, it should be placed in a location where it is easily accessible to EMS personnel and other healthcare providers, such as in the patient's home or on their person if possible. Copies should also be provided to relevant parties, including family members and healthcare proxies, to ensure the order is respected across all care settings.
Is the DNR Order recognized outside of hospital settings?
Yes, in Illinois, the DNR Order is recognized both in hospital settings and by emergency medical services (EMS) outside of hospitals. It's crucial the order is immediately available to emergency personnel, who should respect the wishes documented in the DNR Order.
Are there legal implications for healthcare providers who follow a DNR Order?
Healthcare providers who follow a valid DNR Order are typically protected from legal action regarding their compliance with the order. Illinois law provides immunity to healthcare providers who, in good faith, follow a DNR Order, ensuring that the patient's wishes are honored without placing the provider at risk of legal repercussions.
Common mistakes
In Illinois, filling out a Do Not Resuscitate (DNR) Order form requires attention to detail to ensure one's wishes are clearly stated and legally recognized. A common mistake is not fully understanding what a DNR is. This leads to confusion about when it applies. A DNR Order tells healthcare professionals not to perform CPR if a person's heart stops or if they stop breathing. Without a clear understanding, individuals might not communicate their wishes accurately.
Another oversight is failing to complete the form with all the necessary information. Each section of the DNR form serves a specific purpose, including identifying information, the patient's decision, and the signature of a qualified witness or healthcare provider. Leaving sections incomplete can make the form invalid. This mistake can be easily avoided by carefully reviewing the form and ensuring no section is left blank.
Not having the form signed by the required parties is a critical error. For the DNR Order to be valid, it must be signed by the patient or their legal representative and the patient's physician. Sometimes, people neglect to have their physician review and sign the document, which renders the DNR Order ineffective when it is most needed.
A fourth common mistake involves not discussing the DNR Order with family members or healthcare providers. When individuals do not share their decision with their loved ones or their medical team, it can lead to confusion and distress during emergency situations. This communication ensures that everyone involved understands the patient's wishes and is prepared to respect them.
Last, many people forget to review and update their DNR Orders. As circumstances and perspectives change, it's essential to reconsider previously made decisions. An outdated DNR Order might not reflect a person's current wishes. Regularly reviewing and updating the document as necessary ensures that it accurately represents one's latest healthcare preferences.
Documents used along the form
When preparing for serious health care decisions, particularly those surrounding end-of-life preferences, various documents complement the Illinois Do Not Resuscitate (DNR) Order form. These documents ensure that an individual's wishes are clear and legally recognized. Understanding each document's purpose can guide individuals and their families in comprehensive healthcare planning.
- Power of Attorney for Health Care: This legal document permits an individual to designate another person (agent) to make healthcare decisions on their behalf if they are unable to do so. The agent can also enforce the individual’s wishes regarding the use or non-use of life-sustaining treatments if the individual becomes incapacitated.
- Living Will: A Living Will allows individuals to document their preferences regarding the type of medical care they wish to receive or refuse, particularly in situations where they are terminally ill and unable to communicate their wishes. It often includes directives regarding the use of life-sustaining procedures.
- Physician Orders for Life-Sustaining Treatment (POLST): The POLST form complements a DNR order by providing more comprehensive instructions regarding other forms of life-sustaining treatments beyond resuscitation, such as the use of antibiotics, intubation, and artificial nutrition.
- Five Wishes: Broadening the scope of a living will, the Five Wishes document enables individuals to specify personal, emotional, and spiritual preferences in addition to medical directives. This document helps guide loved ones and healthcare providers in making decisions that align closely with the individual's values and wishes.
- HIPAA Release Form: This form allows healthcare providers to share an individual's medical information with designated persons. It is crucial for the healthcare agent and other loved ones to be fully informed about the individual's medical status and treatment to make informed decisions in line with their wishes.
Comprehensively planning for healthcare and end-of-life scenarios involves more than filling out a Do Not Resuscitate order. By utilizing a combination of these documents, individuals can ensure that their healthcare preferences are well-documented and legally protected, providing peace of mind for both them and their families.
Similar forms
The Illinois Do Not Resuscitate (DNR) Order form is similar to a Living Will in that both documents express an individual’s healthcare preferences in critical situations. A Living Will typically outlines a person’s wishes regarding various life-sustaining treatments when they can no longer communicate their decisions due to incapacitation. Like the DNR Order, it serves as a guide for healthcare providers and loved ones in making decisions that align with the patient's wishes.
Similarly, the Healthcare Power of Attorney (HCPOA) shares commonalities with the DNR Order as it is also a document preparing for a situation where an individual cannot make medical decisions for themselves. While the DNR Order specifically addresses the desire not to have CPR performed, a HCPOA appoints someone else to make a range of healthcare decisions on the individual's behalf. This can include decisions about life-sustaining treatments, indicating a broader authority than the specific instruction found in a DNR.
An Advance Directive is another document closely related to the DNR Order. It combines the elements of a Living Will and a HCPOA, detailing a person’s healthcare preferences and appointing a healthcare proxy. The directive provides comprehensive instructions on the individual’s healthcare wishes, encompassing the refusal of specific treatments like those described in a DNR Order, among other medical considerations.
The Physician Orders for Life-Sustaining Treatment (POLST) form also shares similarities with the DNR Order. The POLST form is designed for individuals facing serious illnesses and details the types of medical treatment they want to receive at the end of their life. Like a DNR, it is medically binding and may include instructions on CPR, ventilation, antibiotic use, and artificial nutrition and hydration.
The Five Wishes document, while broader in scope, relates to the Illinois DNR Order by addressing the issue of medical treatment preferences at the end of life. This document goes beyond medical elements to cover personal, spiritual, and emotional wishes. Although it provides a comprehensive plan that can include DNR instructions, it also facilitates discussions about comfort care, dignity, and communication with loved ones.
The Emergency Medical Services (EMS) Do Not Resuscitate Order is a document used specifically in emergency situations outside of hospital settings, similar to the Illinois DNR Order, which might apply in both inpatient and outpatient contexts. This form instructs emergency personnel not to perform CPR or other life-sustaining treatments. It is designed for individuals with terminal illnesses or severe medical conditions who wish to avoid aggressive measures to prolong their life during an emergency.
Last Will and Testament documents, though primarily focused on the distribution of an individual’s assets after death, relate to the DNR Order in their preparation for end-of-life scenarios. Some individuals might include personal messages or wishes regarding their funeral arrangements and other aspects of their healthcare within these documents. Although not directly concerned with medical interventions, they reflect the individual’s contemplation of mortality and their preferences concerning posthumous matters.
Dos and Don'ts
Filling out the Illinois Do Not Resuscitate (DNR) Order form requires thoughtful consideration and attention to detail. Below are key dos and don'ts that individuals should follow to ensure their wishes are accurately documented and legally recognized.
Do:
- Ensure all information provided on the form is accurate and up-to-date. This includes personal information, medical details, and contact information for a healthcare proxy or next of kin.
- Discuss your decision with a healthcare professional to fully understand the implications and ensure that the DNR order is in line with your healthcare goals.
- Sign and date the form in the presence of a witness or notary, as required by Illinois law, to validate the document.
- Provide copies of the completed DNR order to your primary care physician, family members, and any healthcare proxies or powers of attorney who might need to be aware of your wishes.
- Review and possibly update the DNR order periodically, especially after any major health diagnosis, treatment shift, or change in healthcare preferences.
- Carry an identification that indicates you have a DNR order, such as a bracelet, to ensure that your wishes are known even if you're unable to communicate them.
Don't:
- Leave any section of the form blank. If a question does not apply to your situation, clearly mark it as "N/A" (not applicable) to demonstrate that the omission was intentional.
- Attempt to fill out the form without consulting a healthcare professional. Their guidance is crucial in making informed decisions about end-of-life care.
- Forget to notify close family members or any other individuals who play a significant role in your healthcare decisions. It's important they understand your wishes and the reasons behind them.
- Use ambiguous language. The form should clearly state your wishes regarding resuscitation attempts. Unclear instructions can lead to confusion and potential misapplication of your preferences.
- Fail to keep the original document in a safe, accessible place where it can easily be found in an emergency.
- Assume that the DNR order is universally known without verification. Always confirm with healthcare providers that they are aware of and have documented your DNR status in your medical records.
Misconceptions
When discussing the Illinois Do Not Resuscitate (DNR) Order form, there are several misconceptions that can lead to confusion. Below, ten of these misunderstandings are clarified to provide a better understanding of the form's purpose and use.
- Anyone can sign a DNR Order on behalf of a patient. In fact, only the patient can request a DNR Order, or, if the patient is unable to make their own healthcare decisions, a legally authorized representative such as a power of attorney for healthcare or a guardian can do so.
- A DNR Order is only for the elderly or terminally ill. This misconception overlooks that a DNR Order may be appropriate for patients of any age who wish to avoid resuscitation efforts in the event their heart stops or they stop breathing, based on their personal healthcare goals and conditions.
- DNR Orders are permanent and cannot be changed. On the contrary, a DNR Order can be revised or revoked at any time by the patient or their authorized representative, ensuring that the patient's current wishes are always respected.
- DNR Orders mean no medical treatment will be provided. A DNR Order specifically indicates that CPR should not be initiated in the event of cardiac or respiratory arrest. Patients with a DNR Order still receive all other appropriate medical treatments and interventions.
- Emergency Medical Services (EMS) personnel will not respond to 911 calls if a DNR Order is in place. EMS teams will still respond to emergencies. The DNR Order only guides their actions regarding CPR, not other life-saving measures they are equipped to provide.
- A DNR Order is the same as a living will. These are two different documents. A living will generally outlines a person’s wishes regarding various types of medical treatments in the event they are unable to communicate those wishes themselves, whereas a DNR Order specifically relates to CPR.
- Having a DNR Order means you'll die without being in a hospital. This is not always the case. Patients with a DNR Order may still be hospitalized for various reasons and receive treatments that align with their health care goals, excluding CPR.
- DNR Orders can only be implemented in a hospital setting. DNR Orders are also applicable in non-hospital settings, such as at home or in long-term care facilities, and EMS personnel are trained to recognize and comply with these orders.
- There is a statewide registry for DNR Orders in Illinois. Illinois does not have a statewide registry for DNR Orders, so it’s important for patients to inform their healthcare providers and family about their DNR status and keep copies of the order readily accessible.
- If you have a DNR Order, doctors will not communicate with your family about care decisions. Whether or not a patient has a DNR Order, doctors are still committed to communication with the patient’s family members, as permitted by the patient or applicable law, regarding the patient's care and treatment options.
Key takeaways
Filling out and utilizing the Illinois Do Not Resuscitate (DNR) Order form is an important process requiring careful attention to detail and an understanding of the document's implications. This order communicates a patient's wish not to receive cardiopulmonary resuscitation (CPR) in the event of a cardiac or respiratory arrest. To ensure the DNR order is executed as intended, consider the following key takeaways:
- The DNR order must be completed by a licensed healthcare provider. This includes verifying the patient's diagnosis, prognosis, and desire for the DNR order.
- For a DNR order to be valid, it must be signed by the patient or, if the patient is unable to sign, a legally authorized representative.
- Clear communication between the patient, family members, and healthcare providers is crucial to ensure all parties understand the patient's wishes regarding life-sustaining treatments.
- The completed DNR order should be readily accessible to healthcare providers, ideally included in the patient's medical record and kept in a visible location within the patient's home if home care is being received.
- It's important to review and potentially update the DNR order in response to any significant changes in the patient's health status or treatment preferences.
- Educating patients and families about the implications of a DNR order is a responsibility of the healthcare provider, ensuring informed decisions are made.
- The DNR order is specific to the refusal of CPR and does not impact other treatments or interventions a patient may receive.
- Understanding the legal requirements and protections afforded by the Illinois DNR order helps protect both the patient's wishes and the healthcare providers involved in the patient's care.
Ensuring these elements are addressed can significantly impact the respect and dignity afforded to patients at the end of life, aligning medical care with their wishes and values.
More Do Not Resuscitate Order State Forms
Can a Family Member Override a Dnr - Signing this form can provide peace of mind to individuals wishing to avoid aggressive medical interventions at life's end.
How Old Do You Have to Be to Sign a Dnr - Creating a DNR order involves thoughtful dialogues about values, quality of life, and perspectives on death and dying.
Printable Dnr Form - Advance directives, including DNR Orders, are an important aspect of patient autonomy, allowing individuals to control the decisions about their healthcare and treatment.
Texas Dnr Law - The document ensures that an individual’s choices about end-of-life care are known and respected by healthcare providers.