Fillable Do Not Resuscitate Order Document for Florida
When individuals face serious health conditions, they often confront difficult decisions about the extent of medical interventions they want during emergencies. One such pivotal choice is embodied in the Florida Do Not Resuscitate (DNR) Order form, a legal document that speaks volumes about a person's wishes concerning life-sustaining treatments. This form plays a crucial role in the medical field by ensuring that patients' preferences regarding resuscitation efforts, especially in instances where they cannot communicate their desires, are known and respected. It's not merely a piece of paper but a significant declaration that influences the actions healthcare professionals take in critical moments. The form, recognized by healthcare providers throughout Florida, requires careful consideration and understanding, as it covers major aspects of a person's end-of-life care preferences. Completing the DNR involves a thoughtful discussion with healthcare practitioners and family members to align everyone's understanding and acceptance of the individual's decisions regarding resuscitation.
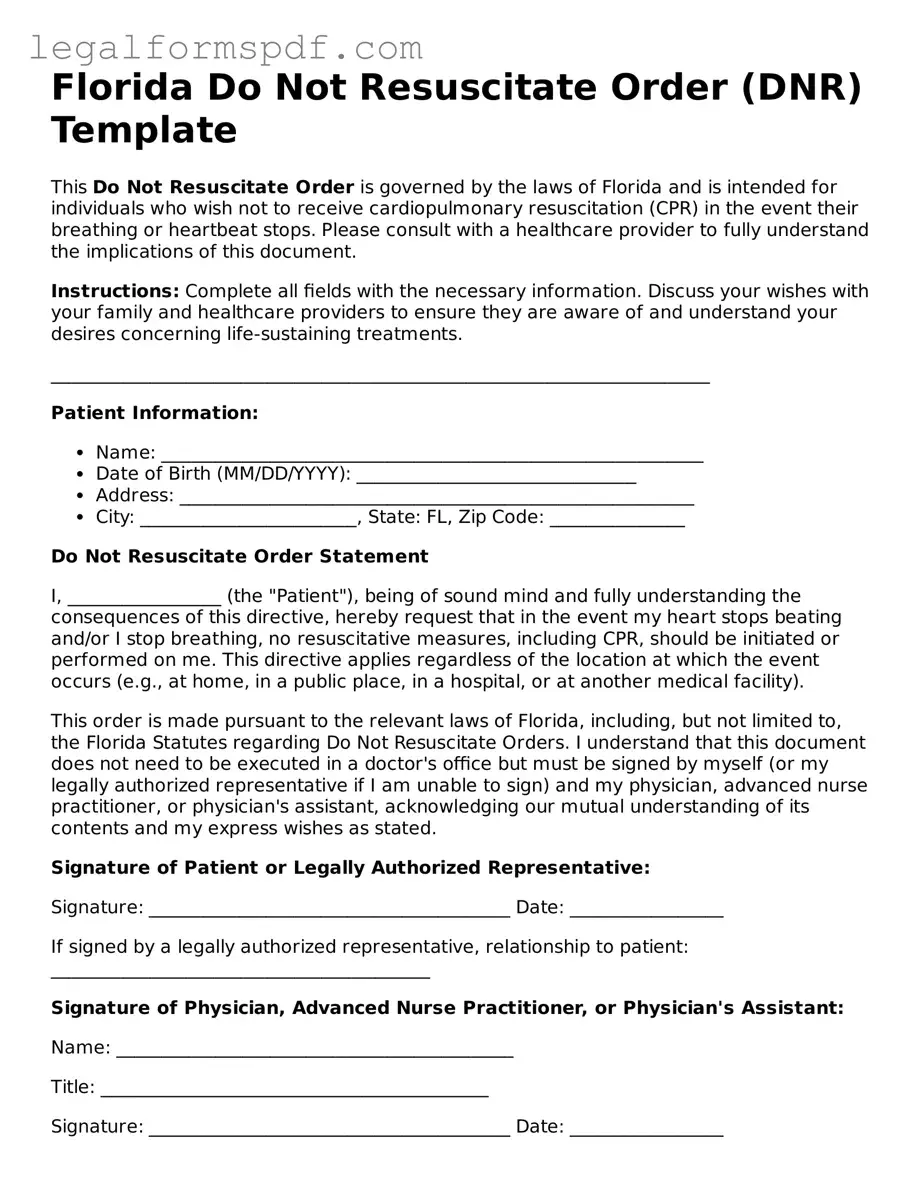
Document Example
Florida Do Not Resuscitate Order (DNR) Template
This Do Not Resuscitate Order is governed by the laws of Florida and is intended for individuals who wish not to receive cardiopulmonary resuscitation (CPR) in the event their breathing or heartbeat stops. Please consult with a healthcare provider to fully understand the implications of this document.
Instructions: Complete all fields with the necessary information. Discuss your wishes with your family and healthcare providers to ensure they are aware of and understand your desires concerning life-sustaining treatments.
_________________________________________________________________________
Patient Information:
- Name: ____________________________________________________________
- Date of Birth (MM/DD/YYYY): _______________________________
- Address: _________________________________________________________
- City: ________________________, State: FL, Zip Code: _______________
Do Not Resuscitate Order Statement
I, _________________ (the "Patient"), being of sound mind and fully understanding the consequences of this directive, hereby request that in the event my heart stops beating and/or I stop breathing, no resuscitative measures, including CPR, should be initiated or performed on me. This directive applies regardless of the location at which the event occurs (e.g., at home, in a public place, in a hospital, or at another medical facility).
This order is made pursuant to the relevant laws of Florida, including, but not limited to, the Florida Statutes regarding Do Not Resuscitate Orders. I understand that this document does not need to be executed in a doctor's office but must be signed by myself (or my legally authorized representative if I am unable to sign) and my physician, advanced nurse practitioner, or physician's assistant, acknowledging our mutual understanding of its contents and my express wishes as stated.
Signature of Patient or Legally Authorized Representative:
Signature: ________________________________________ Date: _________________
If signed by a legally authorized representative, relationship to patient: __________________________________________
Signature of Physician, Advanced Nurse Practitioner, or Physician's Assistant:
Name: ____________________________________________
Title: ___________________________________________
Signature: ________________________________________ Date: _________________
License Number: __________________________________
_________________________________________________________________________
This document should be kept in a location where it can be easily accessed by emergency personnel or healthcare providers. Consider informing close family, friends, and caregivers of the document's existence and location.
Note: This template is provided for informational purposes only and does not constitute legal advice. For personalized advice and to ensure this document meets all legal requirements and accurately reflects your wishes, consider consulting with a legal professional or healthcare provider specialized in end-of-life care decisions.
PDF Specifications
| Fact | Detail |
|---|---|
| Purpose | Specifies a person's wish not to receive cardiopulmonary resuscitation (CPR) in case of a cardiac or respiratory arrest. |
| Applicable Law | Florida Statutes, Section 765.101 - 765.113, known as the "Florida Do Not Resuscitate Order Act". |
| Form Requirement | Must be on yellow paper when printed and utilized in a clinical setting. |
| Signature Requirement | Needs to be signed by the patient (or their legal representative) and the physician. |
| Age Requirement | Person signing must be 18 years or older, or an emancipated minor. |
| Revocation | Can be revoked by the patient at any time, without any specific form or procedure. |
| Recognition | Recognized by healthcare providers across Florida, including hospitals, nursing homes, and emergency medical services. |
Instructions on Writing Florida Do Not Resuscitate Order
Completing the Florida Do Not Resuscitate Order form is a crucial step for those who wish to clearly state their preference not to be resuscitated in case of cardiac or respiratory arrest. This legal document must be filled out accurately to ensure that healthcare providers understand and respect the individual's wishes. The process involves providing personal information, understanding the implications of the form, and obtaining the necessary signatures. Here, we offer a step-by-step guide to help ensure the form is completed correctly.
- Gather Required Information: Before starting the form, collect all necessary personal information including your full name, date of birth, and address.
- Read the Form Carefully: Understanding every part of the form is important. Take your time to read through the entire document to ensure you fully understand the implications of signing it.
- Enter Personal Details: Fill in your personal information in the designated sections. Make sure the information is accurate and matches your official documents.
- Review the Conditions: The form contains specific conditions under which the Do Not Resuscitate Order is applicable. Review these conditions to make sure they align with your wishes.
- Sign the Form: Once you have completed all sections of the form and reviewed it for accuracy, sign the form in the designated area. This signature is your legal agreement to the conditions outlined in the document.
- Obtain Witness Signatures: Florida law may require that one or more witnesses also sign the form, affirming that you signed the document voluntarily and without coercion. Check the most current requirements for witness signatures.
- Consult a Healthcare Professional: It’s advised to discuss the Do Not Resuscitate Order with a healthcare provider or legal professional to ensure its validity and to have it placed in your medical record.
- Make Copies: Keep the original document in a safe but accessible place. Distribute copies to relevant parties, such as family members and healthcare providers, to ensure that your wishes are known.
Completing the Florida Do Not Resuscitate Order form is a proactive way to make your healthcare preferences known and ensure they are respected. By following these steps, you can rest assured that this important document accurately reflects your wishes regarding resuscitation efforts.
Understanding Florida Do Not Resuscitate Order
What is a Do Not Resuscitate Order form in Florida?
A Do Not Resuscitate Order (DNRO) form is a legal document in Florida that tells healthcare providers not to perform cardiopulmonary resuscitation (CPR) if a person's breathing stops or if their heart stops beating. It's used by people who want to decline life-prolonging measures under those circumstances.
Who can request a DNRO in Florida?
In Florida, an adult who is mentally competent can request their own DNRO. If the individual is a minor or not capable of making their own healthcare decisions, a legal guardian or a healthcare surrogate may request the DNRO on their behalf.
How can one get a DNRO form in Florida?
The Florida Department of Health provides the DNRO form, which can be downloaded from their website or obtained from a healthcare provider. The form must be completed as directed to be valid.
Does a doctor need to sign the Florida DNRO form?
Yes, for a DNRO to be valid in Florida, it must be signed by a licensed physician. The physician's signature indicates that they have discussed the implications of the DNRO with the patient (or their representative) and that the patient understands the decision.
Is the DNRO form permanent?
No, a DNRO form is not permanent. The individual or their legal representative can revoke it at any time. Also, the DNRO should be reviewed regularly and especially after any significant change in the individual's health condition.
What happens if emergency medical services (EMS) are not aware of my DNRO?
If EMS personnel are not made aware of your DNRO, they are likely to proceed with all resuscitative measures in an emergency. It's important to keep the DNRO form in an easily accessible location and consider informing close relatives or caretakers of its existence and location.
Does having a DNRO mean I will not receive any medical treatment?
No, having a DNRO does not mean you will be denied medical treatment. It specifically instructs healthcare providers not to perform CPR. You will still receive other forms of medical care unless you have additional directives stating otherwise.
Common mistakes
When faced with the daunting task of making end-of-life decisions, individuals and their families often find solace in establishing a Do Not Resuscitate (DNR) Order. In Florida, this crucial document allows people to express their wishes regarding resuscitation attempts in the event they become critically incapacitated. However, the filing process is fraught with complexities and potential pitfalls. Understanding these common mistakes can help in ensuring that one's healthcare wishes are honored correctly.
One significant error occurs when individuals fail to use the official state form. Florida law requires the use of a specific form for DNR orders to be legally valid. Yet, some people might use an unsanctioned format or draft their own document, thinking it will be recognized. This oversight can render the DNR order ineffective, leaving healthcare providers no choice but to perform lifesaving procedures that the individual might not have wanted.
Another common mistake is not having the form signed by a qualified healthcare provider. The Florida DNR order must be signed by a physician, physician assistant, or advanced practice registered nurse who has assessed the patient's condition and agrees that a DNR order is appropriate. Without this professional endorsement, the document lacks legal standing, which might lead to unwanted medical interventions.
A considerable number of individuals overlook the importance of having the form readily accessible. A DNR order only works if it can be presented to emergency responders or hospital staff in a timely manner. Keeping the document in a safe deposit box or a location where others cannot find it easily defeats its purpose. It is advisable to keep multiple copies in easily accessible places, inform close relatives or friends of its location, and consider carrying a DNR identification bracelet or necklace.
Moreover, some people mistakenly believe that once the DNR order is signed, it is set in stone. However, circumstances and preferences can change, and Florida law allows for the revocation or amendment of a DNR order at any time. Failing to update the DNR order to reflect current wishes can lead to a serious dissonance between what is documented and what the individual truly desires at the end of their life.
Finally, the error of not discussing the decision with family members and medical providers can lead to confusion and conflict. Such conversations ensure that everyone involved is aware of the individual's wishes and understands the reasoning behind them. This collective awareness helps prevent disputes and ensures that the DNR order is respected and implemented as intended.
Navigating the complexities of a DNR order in Florida demands careful attention to detail and a thorough understanding of legal requirements. By avoiding these common mistakes, individuals can ensure that their end-of-life preferences are clearly communicated and respected, providing peace of mind for themselves and their loved ones.
Documents used along the form
When making health care decisions, particularly those concerning end-of-life care, it is imperative to consider various legal documents along with a Do Not Resuscitate (DNR) Order in Florida. These forms ensure that an individual’s healthcare preferences are clearly documented and legally recognized, guiding healthcare providers and relieving the burden on family members during difficult times. Key documents that are frequently used in conjunction with a Florida DNR include the following:
- Living Will: This document allows an individual to outline their preferences for medical treatment in scenarios where they are unable to communicate their wishes. It can specify which, if any, life-prolonging measures they desire.
- Health Care Surrogate Designation: This appoints another person to make health care decisions on the individual's behalf if they are unable to do so. This role can include the decision to implement or withhold the DNR order according to the circumstances.
- Power of Attorney: While similar to a Health Care Surrogate, a Power of Attorney can grant broader authority, including non-healthcare related decisions.
- Limited Power of Attorney for Health Care: This narrows the scope of decision-making authority granted to another individual, focusing specifically on healthcare decisions, including the enforcement of a DNR order.
- Pre-Hospital Do Not Resuscitate Order: This specific form of DNR is designed for emergency medical services personnel, indicating that in the event of a cardiac or respiratory arrest, resuscitation should not be attempted before hospitalization.
- Organ and Tissue Donation Registration: This form specifies an individual's wishes regarding organ and tissue donation after death, which can be an important consideration in end-of-life planning.
- Will: Although not directly related to healthcare decisions, a will is essential in end-of-life planning to direct the distribution of an individual’s assets according to their wishes.
- Five Wishes Document: This combines a living will and health care power of attorney along with personal, emotional, and spiritual wishes to give a comprehensive outline of one’s end-of-life care preferences.
- MOLST (Medical Orders for Life-Sustaining Treatment): In some states, this medical order specifies which treatments a patient wants or doesn’t want at the end of life, including nutrition, intubation, and use of antibiotics, among others.
Together, these documents form a comprehensive approach to end-of-life planning, ensuring that an individual’s healthcare preferences are respected and legally protected. It is advisable for anyone considering a DNR to also explore these additional documents to ensure a holistic approach to their healthcare planning. Consulting with healthcare providers and legal professionals can provide guidance tailored to an individual’s personal wishes and medical situation, making a difficult process more manageable for everyone involved.
Similar forms
The Florida Do Not Resuscitate Order (DNRO) form shares similarities with several other legal documents that are used to guide medical and personal decisions. These documents, though varied in their focus, all play crucial roles in planning for future care, specifying individual wishes, and guiding actions by others when one is unable to communicate their preferences directly.
A Living Will is one such document, quite similar to the DNRO. It allows individuals to outline their wishes for medical treatment should they become unable to make decisions for themselves, particularly regarding life-prolonging measures. While a Living Will speaks to various treatments, the DNRO specifically requests not to be resuscitated in the event of cardiac or respiratory failure.
The Medical Power of Attorney (MPOA) is another pivotal document, appointing someone to make healthcare decisions on behalf of the individual if they're incapacitated. The scope of the MPOA is broader, potentially encompassing all medical decisions, unlike the DNRO's specific refusal of resuscitation efforts.
Then there’s the Durable Power of Attorney for Finances, analogous in that it designates a person to handle one's financial affairs under certain conditions. It parallels the DNRO as a preparatory action, ensuring a trusted individual has the authority to act in one's best interest, albeit in a financial rather than medical context.
The POLST (Physician Orders for Life-Sustaining Treatment) form also shares common ground with the DNRO. It details specific instructions about life-sustaining treatments for those with serious illnesses. Unlike the DNRO, which is exclusively about non-resuscitation, the POLST covers a broader range of medical interventions.
A Health Care Surrogate Designation is a document appointing another person to make healthcare decisions when the principal cannot. It covers decisions beyond DNR instructions, allowing the surrogate to make a wider range of medical decisions than the DNRO permits.
The Advance Directive is a broader term that encompasses different types of healthcare directives, including a Living Will and a Medical Power of Attorney. It serves as a comprehensive document to communicate an individual's wishes about medical treatment, of which a DNRO might be considered a very specific component.
Lastly, a Last Will and Testament, while principally addressing the distribution of an individual's estate after their death, shares a fundamental similarity with the DNRO: both are preparatory documents, articulating wishes that are to be respected and executed upon the individual's death or near-death condition.
Each of these documents, though distinct in its primary function, is integral to comprehensive life planning, addressing different facets of a person's wishes for the time when they may not be able to express those wishes themselves. The DNRO, alongside these other documents, ensures that individuals have control over their end-of-life care, financial matters, and health care decisions, promoting dignity and respect for their choices.
Dos and Don'ts
Filling out the Florida Do Not Resuscitate Order (DNRO) form properly is critical for ensuring that a patient's wishes regarding life-prolonging procedures are respected in critical situations. Below are ten vital do's and don'ts to consider when completing this important document.
Do:
- Verify that the patient or their legally recognized health care surrogate is the one completing the form. It ensures the authenticity and legality of the document.
- Ensure that the form is signed by a Florida-licensed physician. This is a requirement for the DNRO to be considered valid.
- Use the patient's legal name to avoid any confusion or discrepancies with other legal documents or identification.
- Discuss the implications of the DNRO with the patient's healthcare provider to make an informed decision. Understanding the consequences of not performing resuscitation can give clarity.
- Include the date on which the DNRO is signed to maintain a clear record of when the order was made, aiding in its enforceability.
Don't:
- Leave any fields incomplete. An incomplete form may not be legally binding, potentially leading to the administration of unwanted medical treatments.
- Allow anyone other than the patient, their surrogate, or a Florida-licensed physician to sign the form. Doing so could invalidate the document.
- Falsify any information. This could lead to legal consequences and compromise the patient's health care wishes.
- Laminate or alter the original document after it has been completed and signed. Such changes can cast doubt on the validity of the order.
- Forget to review and, if necessary, update the DNRO periodically. Circumstances and wishes can change, necessitating a review to ensure the document reflects the patient's current desires.
Misconceptions
Many people have misunderstandings about the Florida Do Not Resuscitate Order (DNRO) form. These misconceptions often stem from lack of information or confusion about the state’s laws and health care directives. Below are four common misconceptions about the Florida DNRO form, explained to help clarify their true aspects.
All medical treatments are halted with a DNRO form. A common misconception is that by signing a DNRO, a person is refusing all medical treatments. This is not the case. The DNRO specifically applies to cardiopulmonary resuscitation (CPR) in the event that someone's breathing stops or their heart stops beating. It does not affect other treatments the patient may receive for pain relief, injury, or illness.
Anyone can create or sign a DNRO on behalf of the patient. In Florida, the rules are strict about who can consent to a DNRO. The individual must be of sound mind to make this decision for themselves or, if they are not able to, a legally authorized representative (such as a healthcare surrogate) can do so on their behalf. This emphasizes the importance of clear communication and legal authority in health care decisions.
The Florida DNRO is recognized in all states. This is a widespread misunderstanding. While many states have their form of Do Not Resuscitate orders, and healthcare professionals generally respect patients' wishes, the Florida DNRO is not automatically valid in other states. Each state has its own laws and forms regarding Do Not Resuscitate orders. Individuals moving or traveling should consult with legal and medical professionals about their state's recognition of out-of-state DNRO documents.
Once signed, the DNRO cannot be revised or revoked. Another misconception is that once a DNRO form is signed, it is permanent. In reality, a patient or their authorized representative can revoke or modify the DNRO at any time. This decision can be based on a change in the patient's health condition or a change in their wishes about end-of-life care. It's crucial for patients and families to understand that they have the right to change these important health care directives as circumstances change.
Key takeaways
When considering the completion and application of the Florida Do Not Resuscitate (DNR) Order form, which allows individuals to decline resuscitation in the event of respiratory or cardiac arrest, it's important to approach the matter with both understanding and sensitivity. The purpose of this documentation is not just procedural but deeply personal, ensuring that a person's medical and end-of-life wishes are respected. Below are key takeaways designed to provide clarity and guidance through this critical process:
- Valid Execution: The DNR Order must be completed accurately to ensure it's legally valid. This includes obtaining the necessary signatures from the individual or their legally authorized representative, as well as a Florida-licensed physician, osteopathic physician, or advanced practice registered nurse (APRN).
- Comprehension is Critical: Before signing, the person must fully understand the implications of a DNR Order, which means that they are choosing not to receive CPR (cardiopulmonary resuscitation) in the event of cardiac or respiratory arrest.
- Physician Responsibilities: The healthcare provider signing the form assumes responsibility for ensuring the individual (or their representative) comprehends the nature and scope of the DNR Order.
- Form Accessibility: The DNR Order should be kept in an easily accessible location so that it can be promptly presented to emergency medical personnel or healthcare providers when necessary.
- Durability of the Order: It's essential to know that the DNR Order is valid unless revoked. The individual has the right to revoke the order at any time, which should be done in a clear and understandable manner.
- Recognition Across Various Settings: While primarily intended for emergency medical services personnel, the DNR Order is recognized across different healthcare settings. It's pertinent in hospitals, nursing homes, and in the home.
- Replication of the Document: It is advisable to have multiple copies of the DNR Order. Originals or copies should be readily available for presenting to emergency or healthcare personnel when needed.
- Traveling with a DNR Order: For those who frequently travel away from home, carrying a copy of the DNR Order or wearing a DNR identification, such as a bracelet, can ensure that your wishes are respected, even outside of your primary residence.
- Legal and Medical Consultation: Considering the significance of a DNR Order, consulting with healthcare and legal professionals can provide valuable guidance. They can help clarify any uncertainties about the form and its implications for individual healthcare wishes and obligations.
Understanding and filling out the Florida Do Not Resuscitate Order form is a profound decision, warranting thoughtful consideration and discussions with loved ones and professionals. It's about ensuring that personal wishes are respected, emphasizing autonomy and dignity at a critical time.
More Do Not Resuscitate Order State Forms
Il Polst Form - In emergency situations where EMTs or emergency medical personnel are called, the presence of a Do Not Resuscitate Order informs their actions.
Dnr Form Ohio - A binding legal instrument that clearly states an individual's decision to decline CPR or advanced cardiac life support.
Does a Dnr Need to Be Notarized in California - While a DNR focuses primarily on not initiating CPR, it does not mean other forms of palliative care will be withheld, such as pain management and comfort measures.