Official Do Not Resuscitate Order Document
When individuals approach the complexities of life and health, certain decisions must be carefully considered, especially regarding medical interventions at the end of life. Among these critical choices is the Do Not Resuscitate (DNR) Order form, a document that holds significant weight and influence over the course of a patient's medical treatment. Essentially, this form allows a person to express their wish not to undergo CPR (cardiopulmonary resuscitation) or other life-saving measures in the event their heart stops or they stop breathing. This decision is deeply personal and can reflect a variety of factors, including the individual's values, beliefs, medical conditions, and quality of life considerations. Healthcare professionals must respect the stipulations of a DNR order, thus making it an essential component of end-of-life planning. It navigates the delicate balance between the right to make autonomous health care decisions and the complex ethical, medical, and emotional issues surrounding death and dying. The process of completing a DNR form involves thoughtful discussion with healthcare providers and often, family members, to ensure that the individual’s wishes are clearly understood and documented.
State-specific Information for Do Not Resuscitate Order Forms
Document Example
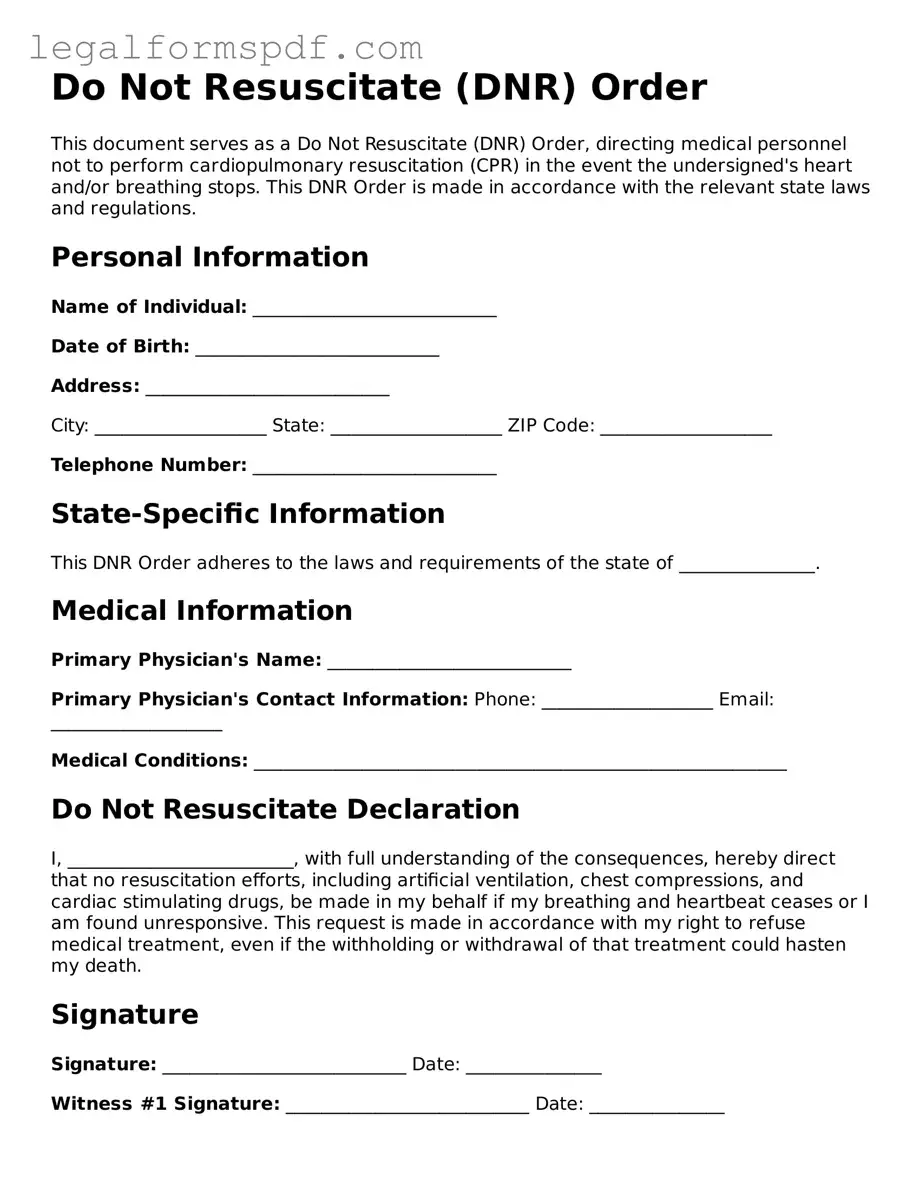
Do Not Resuscitate (DNR) Order
This document serves as a Do Not Resuscitate (DNR) Order, directing medical personnel not to perform cardiopulmonary resuscitation (CPR) in the event the undersigned's heart and/or breathing stops. This DNR Order is made in accordance with the relevant state laws and regulations.
Personal Information
Name of Individual: ___________________________
Date of Birth: ___________________________
Address: ___________________________
City: ___________________ State: ___________________ ZIP Code: ___________________
Telephone Number: ___________________________
State-Specific Information
This DNR Order adheres to the laws and requirements of the state of _______________.
Medical Information
Primary Physician's Name: ___________________________
Primary Physician's Contact Information: Phone: ___________________ Email: ___________________
Medical Conditions: ___________________________________________________________
Do Not Resuscitate Declaration
I, _________________________, with full understanding of the consequences, hereby direct that no resuscitation efforts, including artificial ventilation, chest compressions, and cardiac stimulating drugs, be made in my behalf if my breathing and heartbeat ceases or I am found unresponsive. This request is made in accordance with my right to refuse medical treatment, even if the withholding or withdrawal of that treatment could hasten my death.
Signature
Signature: ___________________________ Date: _______________
Witness #1 Signature: ___________________________ Date: _______________
Witness #1 Printed Name: ___________________________
Witness #2 Signature: ___________________________ Date: _______________
Witness #2 Printed Name: ___________________________
Physician's Statement
I, _________________________ (Physician's Name), license number ________________, hereby confirm that I have discussed the nature and effect of a Do Not Resuscitate Order with the individual or their legally authorized representative. This individual/representative has been informed of their medical condition and the potential consequences of this DNR order.
Physician's Signature: ___________________________ Date: _______________
Important Notes
- This DNR Order is valid immediately upon signing and remains in effect indefinitely unless revoked by the individual or their legally authorized representative.
- A copy of this DNR Order should be provided to the individual’s primary physician, hospital, and/or nursing home where the individual receives care.
- The effectiveness and requirements of DNR Orders may vary by state. It is crucial to consult with legal and medical professionals to ensure compliance with state-specific regulations.
PDF Specifications
| Fact Name | Description |
|---|---|
| Purpose of the Do Not Resuscitate Order | A Do Not Resuscitate (DNR) order is a legal directive in the United States that indicates a person's wish to decline CPR (cardiopulmonary resuscitation) or advanced cardiac life support in case their heart stops or they stop breathing. This is designed to respect the patient's wishes regarding end-of-life care. |
| Form Requirement | DNR orders must be written documents, signed by a healthcare provider and, in most cases, by the patient or their authorized health care proxy or surrogate decision-maker. The form may require specific wording and formats according to state law. |
| State-Specific Laws | Each state in the US has its own laws governing DNR orders. These laws dictate the form's format, the signing process, and how the DNR order is implemented within medical facilities and by emergency personnel. |
| Validity Across Settings | While a DNR order is generally recognized across different healthcare settings within a state, its validity outside of the state where it was issued can vary. Some states have reciprocity agreements or laws that recognize DNR orders from other states, but this is not universal. |
| Revocation | A DNR order can be revoked at any time by the patient if they are mentally competent, or by their authorized representative. This revocation can be done verbally or in writing, depending on the state's requirements. |
Instructions on Writing Do Not Resuscitate Order
A Do Not Resuscitate (DNR) order form is a crucial document for those who wish to decline life-saving measures, such as CPR, in the event their heart stops or they stop breathing. This decision is deeply personal and can be based on a variety of health and ethical reasons. Completing a DNR form properly is essential to ensure your medical wishes are honored. Here are step-by-step instructions to guide you through filling out a DNR order form.
- Begin by gathering personal identification information, including your full legal name, date of birth, social security number, and address. This information is essential to identify you clearly.
- Read the form carefully. Understanding every part of the DNR order form is crucial before you start filling it out to make sure your wishes are accurately captured.
- Enter your personal identification information in the designated sections of the form.
- If the form requires, detail your specific medical conditions or reasoning for choosing a DNR order. Some forms may not have this section.
- Look for the section on the form that requires the signature of a legal witness or witnesses. The requirements can vary by state, so understanding the specific needs for witness signatures in your area is important.
- Sign the DNR order form yourself in the designated area. Note that if you are unable to sign, some states allow for an authorized representative to sign on your behalf. Check your local regulations.
- Have the required witnesses sign the form in their designated areas, if applicable.
- In many cases, a physician's signature is also required on the DNR form. Arrange for your physician to review and sign the form, acknowledging they have discussed the DNR order with you and agree it's in your best interest based on your medical condition.
- After the form is fully completed and signed, make several copies. Provide one to your physician to be included in your medical records, keep another for yourself, and consider giving copies to close family members or your legal representative.
After completing the DNR form, your next steps include discussing your decision with loved ones and ensuring that all relevant parties have a copy or know where to find it. It's also wise to regularly review and update it as needed, especially if your health condition changes. Remember, completing a DNR is a significant decision that requires careful thought and consideration.
Understanding Do Not Resuscitate Order
What is a Do Not Resuscitate (DNR) Order?
A Do Not Resuscitate Order is a legal document that tells healthcare providers not to perform CPR (cardiopulmonary resuscitation) if a person's breathing stops or if their heart stops beating. It is used to respect the patient's wishes not to receive these specific life-saving measures.
Who can request a DNR Order?
Any competent adult can request a DNR Order for themselves. Additionally, legal guardians or healthcare proxies may request a DNR Order on behalf of someone who is not able to make their own medical decisions.
How does one get a DNR Order?
Obtaining a DNR Order usually involves discussing your wishes with your healthcare provider. They can then help fill out the necessary form or provide guidance on how to obtain one. The process may vary slightly from state to state.
Is a DNR Order the same as an advance directive?
No, a DNR Order is not the same as an advance directive. An advance directive is a broader document that can contain a variety of wishes regarding a person's healthcare, including end-of-life care, whereas a DNR specifically deals with not receiving CPR.
Can a DNR Order be revoked?
Yes, a DNR Order can be revoked at any time by the person who requested it, either verbally or in writing, depending on the state's requirements. It's important to communicate this decision to your healthcare provider right away.
What happens if medical staff isn't aware of a DNR Order?
If medical staff are not aware of a DNR Order, they will typically proceed with all life-saving measures, including CPR, in an emergency situation. This highlights the importance of making sure your healthcare providers and loved ones are aware of your DNR Order and its location.
Does a DNR Order need to be renewed?
The need to renew a DNR Order varies by state. Some states require renewal after a certain period, while others do not. It's crucial to check the regulations in your state and keep your DNR Order up to date.
Will a DNR Order be honored in a different state?
Since laws regarding DNR Orders can vary from state to state, there's no guarantee a DNR Order will be recognized in a different state. It's advisable to check the laws of the state you are visiting or relocating to.
What should you do with your DNR Order once it's completed?
Once a DNR Order is completed, keep the original document in a safe but easily accessible place. Make sure to inform your family members, healthcare proxy, and healthcare providers about its existence and location. It's also a good idea to carry a wallet card indicating you have a DNR Order.
Does having a DNR Order affect the quality of care one receives?
No, having a DNR Order does not affect the quality of care a person receives. Healthcare providers will continue to offer all other appropriate treatments and services. The DNR Order specifically applies to the use of CPR and other resuscitative measures only.
Common mistakes
Filling out a Do Not Resuscitate (DNR) order is a significant decision that requires careful consideration and understanding of the document. However, people often make mistakes when completing this form, largely due to a lack of information or understanding of its implications. One common mistake is not discussing their wishes with family members or healthcare providers beforehand. This conversation is crucial as it ensures that ones' desires are fully understood and can be confidently carried out by those who may need to act on the DNR order.
Another frequent error is the failure to properly complete all necessary sections of the form. A DNR form is a legal document that must be filled out accurately to be considered valid. Skipping sections or filling out the form incorrectly can render it ineffective, leading to unwanted medical interventions. It is important to read each section carefully and seek clarification if any part of the form is not understood.
Additionally, many people fail to update their DNR order. Medical wishes and personal circumstances can change over time, but individuals often forget to review and revise their DNR orders to reflect these changes. An outdated DNR order may no longer represent a person's current wishes, causing confusion and distress during critical moments. Regularly reviewing and updating the DNR order can prevent this issue.
Lastly, there is the mistake of not storing the DNR order properly. After going through the process of filling out a DNR order, it should be kept in an easily accessible location and shared with relevant parties, such as family members and healthcare providers. If the DNR order is not readily available when needed, medical staff may proceed with resuscitation efforts against the person's wishes. Ensuring that the document is both visible and accessible can avoid such situations.
Avoiding these mistakes requires awareness, careful planning, and open communication. By addressing these points, individuals can ensure that their healthcare wishes are understood and respected.
Documents used along the form
End-of-life decisions are deeply personal and can be complex to navigate. The Do Not Resuscitate (DNR) Order form is one such directive that is crucial for individuals who wish to decline certain life-sustaining treatments. Alongside a DNR, there are various other legal documents that can support and clarify a person’s healthcare and end-of-life wishes. Each document serves its own purpose and complements the instructions laid out in a DNR Order. Understanding these can ensure more comprehensive planning for oneself or for loved ones.
- Advance Directive: This document allows individuals to outline their healthcare preferences, including decisions about life-sustaining treatment, in the event they cannot communicate. It may also designate a healthcare proxy to make decisions on their behalf.
- Living Will: Closely related to an Advance Directive, a Living Will specifies an individual's preferences regarding the types of medical care they do or do not wish to receive towards the end of life. It can be particularly useful in guiding healthcare providers when a DNR is in place.
- Healthcare Power of Attorney (POA): This appoints a trusted person to make healthcare decisions on behalf of the individual if they are unable to do so. This role can include the authority to enforce or revoke a DNR Order.
- Durable Power of Attorney for Finances: While not related to healthcare decisions directly, this appoints someone to handle financial affairs and can be crucial in ensuring that healthcare needs are funded and financial obligations are met.
- Medical Orders for Life-Sustaining Treatment (MOLST) or Physician Orders for Life-Sustaining Treatment (POLST): These forms are similar to a DNR but offer more detailed instructions about other treatments, such as antibiotics, intensive care, and feeding tubes.
- Organ and Tissue Donation form: Allows individuals to specify their wishes regarding organ donation. This can either be a standalone form or part of one's driver's license registration process in many states.
- Funeral Planning Declaration: Helps individuals specify their preferences for funeral arrangements, such as burial or cremation, type of ceremony, and so on, easing decision-making for families during a difficult time.
- Last Will and Testament: Though primarily focused on the disposition of one's estate after death, a Last Will can also convey one's wishes about certain personal matters and can complement end-of-life care instructions provided in other documents.
- HIPAA Authorization Form: Permits healthcare providers to discuss an individual’s medical condition and share medical records with designated persons, ensuring loved ones can stay informed and make well-informed decisions when necessary.
Each of these documents plays a unique role in a person’s healthcare and end-of-life planning. Together with a Do Not Resuscitate Order, they ensure a person's wishes are understood and respected. It’s advised to consult with a legal professional who can help navigate the creation and implementation of these documents, ensuring that an individual's rights and desires are accurately represented and legally protected.
Similar forms
A living will is a document that shares similarities with a Do Not Resuscitate (DNR) Order, as it also dictates medical wishes in advance. While a DNR specifically directs healthcare providers not to perform CPR in the event of cardiac or respiratory arrest, a living will encompasses a broader range of medical treatments and life-sustaining measures one might wish to decline or accept in scenarios of severe illness or near the end of life. This document communicates a person's decisions regarding healthcare interventions, should they become incapable of making these decisions themselves.
A healthcare power of attorney (POA) designates an individual to make healthcare decisions on someone's behalf if they are unable to do so themselves, akin to the purpose behind a DNR Order. The difference lies in the fact that a healthcare POA covers a wide array of medical decisions, not limited to the acceptance or refusal of life-sustaining treatments. This appointed decision-maker can respond to medical situations as they arise, relying on their understanding of the patient’s wishes and best interests.
The POLST (Physician Orders for Life-Sustaining Treatment) form closely relates to a DNR order by providing specific instructions on a range of life-sustaining treatments according to a patient's wishes. Unlike a DNR, which strictly addresses the use of CPR, a POLST covers more exhaustive ground, detailing preferences for interventions like intubation, mechanical ventilation, and artificial nutrition. POLST forms are intended for those with serious health conditions, turning a patient's treatment preferences into medical orders.
An advance directive is an overarching term that includes documents like living wills and DNR orders. It denotes any legal paperwork that outlines a person’s healthcare wishes in case they are incapacitated. The documents under this label provide instructions on a person’s preferences for medical treatments, including refusal of certain procedures, mirroring the DNR's role in conveying choices about life-sustaining measures. These directives are crucial for guiding loved ones and healthcare providers in decision-making during critical times.
A medical order for life-sustaining treatment (MOLST) form shares similarities with a DNR in that it translates a patient’s preferences regarding end-of-life care and other critical healthcare decisions into actionable medical orders. MOLST forms encompass a broader range of directives, including but not limited to resuscitation instructions, offering a comprehensive strategy for managing a person's medical care when they are facing severe or terminal illness. This form provides clarity and guidance to healthcare teams, ensuring that a patient’s wishes are respected and followed.
The Five Wishes document extends beyond the traditional scope of a DNR by addressing personal, emotional, and spiritual needs alongside medical wishes. It allows individuals to detail their preferences concerning their comfort, how they want to be treated, what they want their loved ones to know, and more, in addition to specifying medical treatments they want to avoid or receive at the end of life. This holistic approach to advance care planning ensures that all aspects of a person’s well-being are considered and honored.
A do not intubate (DNI) order is a specific directive that, like a DNR, is intended to prevent a particular medical intervention—in this case, the insertion of a tube to help with breathing. Both DNR and DNI orders specify interventions to be avoided by healthcare providers when a patient cannot make their own medical decisions. However, while a DNR focuses on the act of resuscitation, a DNI addresses a different aspect of life-saving measures, illustrating the varied nature of treatment preferences an individual can express.
An emergency medical information form is designed to provide first responders and medical personnel with quick access to a person’s critical health information during an emergency. Similar to a DNR, this form can include important instructions regarding the patient’s wishes for emergency medical care. However, it covers a wider range of information, such as medical conditions, allergies, medications, and contacts for next of kin. This comprehensive approach ensures that emergency healthcare providers have a broader understanding of the patient’s health background and wishes.
Dos and Don'ts
When filling out a Do Not Resuscitate (DNR) Order form, there are specific actions you should take to ensure the document is valid and reflects your or your loved one's wishes accurately. Equally important, certain mistakes should be avoided to prevent future complications or misunderstandings. Below are key dos and don'ts to consider:
Do:- Consult with a healthcare provider before completing the form to understand the implications and ensure it reflects the patient’s wishes.
- Ensure that the form is filled out completely, including all required signatures.
- Discuss the decision with close family members or loved ones to ensure they understand the patient’s wishes.
- Keep the completed form in a easily accessible place and inform family members or caretakers of its location.
- Provide copies of the completed form to the patient’s healthcare providers, including the family doctor, specialists, and hospital personnel involved in the patient’s care.
- Review and update the form periodically, especially if the patient’s health status or wishes change.
- Consider wearing a DNR bracelet or carrying a card in your wallet indicating the existence of a DNR order for emergency situations.
- Make sure that the form complies with state laws, as requirements can vary significantly.
- Fill out the form without a thorough discussion with the patient (if capable) and their healthcare provider about the implications.
- Leave sections of the form blank or incomplete, as this can lead to confusion or invalidate the form.
- Fail to communicate the existence of the form to family members and healthcare providers, which could lead to unwanted resuscitation efforts.
- Forget to review and update the form, especially after significant changes in the patient’s health condition.
- Assume that a DNR order is universally recognized; carry proof of the order when traveling or when in unfamiliar medical facilities.
- Store the form in a location where it is difficult for family or emergency personnel to find in a timely manner.
- Overlook the need for additional documentation that may be required, such as power of attorney for healthcare decisions.
- Ignore state-specific forms and regulations, as using the wrong form could render the DNR order ineffective.
Misconceptions
Do Not Resuscitate (DNR) orders are critical documents in healthcare, directing medical professionals on the wishes of a patient regarding resuscitation efforts. However, misconceptions about DNR orders can lead to confusion and distress. Here are nine common myths debunked to clarify what these orders mean and how they work.
- Misconception 1: DNR orders mean no medical treatment.
This is not true. DNR orders specifically address the use of CPR or advanced cardiac life support in the event of cardiac or respiratory arrest. Patients with DNR orders will still receive all other appropriate treatments and comfort care, including pain management and antibiotics, if desired.
- Misconception 2: Only elderly patients can have DNR orders.
Age is not a criterion for a DNR order. These orders apply to anyone, regardless of age, who does not wish to have CPR or advanced resuscitation efforts if their heart or breathing stops.
- Misconception 3: A DNR order must be signed by a family member.
A DNR order is a decision that should reflect the patient's wishes. While the conversation with family members is important, the document must be signed by the patient (if they are competent), or otherwise, a legally authorized representative or healthcare proxy designated by the patient.
- Misconception 4: DNR orders are irreversible.
DNR orders can be revoked or modified at any time by the patient or their legally authorized representative. Patients can always change their minds.
- Misconception 5: Emergency teams will consult the DNR order before taking action.
In an emergency, medical teams often act quickly to save a life, and there may not be time to consult a DNR order, especially if it is not immediately available. For this reason, it is crucial to have the DNR easily accessible and communicate its existence to all caregivers and health professionals involved.
- Misconception 6: DNR orders are mandatory for terminally ill patients.
Deciding to sign a DNR order is voluntary and personal. A patient with a terminal illness might choose to have a DNR order, but it is not a requirement. The decision should be based on individual beliefs, values, and medical advice.
- Misconception 7: A DNR order affects the quality of the rest of the patient's care.
Having a DNR order does not mean that the medical staff will provide less care. It is a specific instruction about resuscitation and does not impact other treatments or the quality of care provided.
- Misconception 8: DNR orders are only valid in hospitals.
While the process for enacting DNR orders may differ between hospitals, nursing homes, and home care, DNR orders are legally valid in all healthcare settings. However, it is essential to make sure that the document is accessible and that its existence is communicated to all healthcare providers involved.
- Misconception 9: Having a DNR order means you are giving up on life.
Choosing a DNR order is a personal decision that can reflect a variety of beliefs, values, and medical considerations. It does not mean giving up but rather a decision about the type of care and interventions a person wants at the end of life or in a critical condition.
Key takeaways
A Do Not Resuscitate (DNR) Order is a critical medical directive that tells healthcare providers not to perform cardiopulmonary resuscitation (CPR) if a person's breathing or heartbeat stops. Here are key takeaways to consider when filling out and using this form:
- Understanding the purpose: A DNR Order is specifically designed for individuals who wish to avoid aggressive life-saving measures in certain medical situations. It is crucial for people who want to have control over their end-of-life care.
- Consult with a healthcare provider: Before completing a DNR Form, the individual or their legal representative should consult with a healthcare provider to fully understand the implications and ensure it aligns with the person’s wishes.
- Proper documentation is essential: The DNR Order must be properly filled out and signed by the required parties, which usually includes the patient (or their legal representative) and the attending physician to be legally valid.
- State laws vary: DNR Orders are subject to varying state laws and regulations. What’s applicable in one state may not be in another, so it's important to be familiar with local requirements.
- Accessibility of the form: Once completed, the DNR Order should be kept in an easily accessible place so that it can be promptly presented to healthcare providers or emergency responders when needed.
- Discussing with family and care team: It’s recommended to discuss the decision to have a DNR Order with family members and the healthcare team to ensure everyone understands the individual’s wishes.
- Regular review and updates: Circumstances and decisions might change. Therefore, the DNR Order should be reviewed periodically and updated as needed to reflect current wishes.
- Impact on other medical treatments: Having a DNR Order does not affect the quality of other medical treatments provided. Patients with a DNR Order still receive comprehensive medical care, minus the efforts to resuscitate.
- Different from a living will: It’s important to distinguish between a DNR Order and a living will. A DNR is specifically focused on CPR and does not address other medical treatments or conditions.
- Incorporating into medical records: The DNR Order should be incorporated into the individual's medical records to ensure that it is respected by all healthcare professionals involved in the person’s care.
Every individual has the right to make decisions about their medical care, including the choice to decline certain treatments such as CPR. Understanding and properly implementing a DNR Order can ensure that these wishes are respected during critical moments.
Other Templates
Hold Harmless Clause - Essential for event planning, it shields organizers from liabilities related to third-party vendors or participants.
Joint Tenancy in California - It is particularly useful in situations where the deceased owned property in a state different from their domicile.
Simple Loan Agreement Template - Featuring a severability clause ensures that if one part of the agreement is found to be unenforceable, the rest of the agreement still remains in effect.